Frozen Shoulder
Lennard Funk, 2007
Introduction:
Frozen shoulder is an extremely disabling condition, presenting with and remitting shoulder pain and stiffness. This was well defined by Codman in 1934, who described the first and best classical diagnostic criteria still used to this day.
These were:
1. Global restriction of shoulder movement.
2. Idiopathic etiology.
3. Usually painful at the outset.
4. Normal x-ray.
5. Limitation of external rotation and elevation.
The classification of a primary idiopathic frozen shoulder may be primary or idiopathic. This is a distinct pathological condition identified by global limitation of glenohumeral motion, with a loss of compliance of the shoulder capsule, with no specific underlying cause found.
A secondary stiff shoulder or secondary frozen shoulder, typically presents after injury or surgery. It may also follow an accompanying condition, such as subacromial impingement or a rotator cuff tear.
Diagnosis:
The diagnosis of a primary Idiopathic frozen shoulder is made on the basis of:
- Age: Typically occurring in females more common than males, in the 4th and 5th decade.
- Pain: The pain is of a constant nature, severe, affecting sleep. There is often a toothache pain at rest, with sharp pains with forceful movements.
- Loss of external rotation: The typical loss of external rotation is such that passive external rotation is <0 degrees from the sagittal plane. A secondary frozen shoulder usually has restriction of external rotation, which is beyond 0 degrees (i.e. external rotation of 10 degrees as opposed to -10 degrees with a primary frozen shoulder).
Natural History:
The natural history of a frozen shoulder has typically been described as passing through 3 stages. These stages last for approximately 2 years.
Stage:
1. Freezing phrase: This is associated with pain and loss for about 3 months.
2. Frozen phase: This lasts for approximately 3-9 months, with pain at extreme range of movement and marked stiffness.
3. Thawing phase: This last for approximately 9-18 months, usually painless and the stiffness starts to gradual resolve at this stage.
The frozen shoulder has been found to be more common in association with the following conditions:
- Diabetes (10-20% association). There is a 2-4 times increased risk for diabetics of developing frozen shoulder. Insulin-dependent diabetics have a 36% chance of developing it, 10% bilaterally and the condition is more severe in diabetics.
- Cardiac/lipid problems.
- Epilepsy.
- Endocrine abnormalities, particularly hypothyroidism.
- Trauma.
- Drugs - MMPI.
The macroscopic appearance is that of thickening of the anterior capsule, particularly the coracohumeral ligament (CHL) and middle glenohumeral ligament MGHL).
Contracture of the capsular ligament restricts specific movements of the glenohumeral joint. These are:
- CHL = external rotation in neutral
- MGHL = external rotation in mid-elevation
- AIGHL = external rotation in abduction
- Inferior capsule (ICS) = abduction in neutral rotation
- PIC = internal rotation
- PSC = internal rotation in abduction
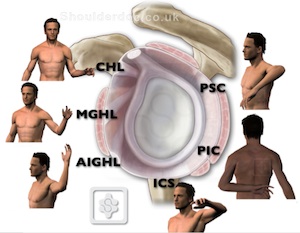
Villonodular synovitis within the rotator interval with thickening and contracture of the coracohumeral ligament is the primary pathology.
The capsular thickening and contracture leads to a reduced glenohumeral joint volume.
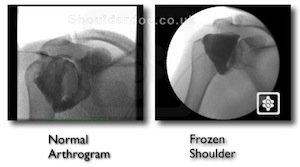
Arthroscopic images showing a normal shoulder on the left, and a frozen shoulder on the right (note the villonodular synovitis):

Arthrogram of a normal shoulder (left) and a frozen shoulder (right) - note the reduced capsular volume:
 Microscopically there are 4 stages:
Microscopically there are 4 stages:
- Inflammatory synovitis with capsule unaffected.
- Proliferative synovitis, which is hypertrophic.
- Maturation of the capsule, with reduced vascularity.
- Burnt out synovium with a dense scar appearance.
Tim Bunker in 1995 has shown the pathology to be similar to Dupuytren's disease with increased collagen, myofibroblast and fibroplasia. This in association with Trisomy 7 & 8, 58% of patients who had a primary idiopathic frozen shoulder had Dupuytren's disease elsewhere. The inflammatory drivers for Dupuytren's disease and frozen shoulder are similar, these being TGF-beta and PDGF.
Treatments:
The natural history of frozen shoulder is not necessarily that of complete resolution. The original quotation that most recover from frozen shoulder originates from Codman in 1934. However, he stated that most frozen shoulders recover compared to tuberculosis. Many studies have shown frozen shoulder not to be an entirely self limiting condition and most patients still have some restriction of shoulder movement on resolution of the frozen shoulder but no functional disability (Grey JBJSA 1962, Shaffer JBJSA 1992, Bunker JBJSB 1995, Miller Orthopaedics 1996).
The treatment options range from:
1. Nothing.
2. Physiotherapy.
3. Distention injections.
4. Locally acting steroid injections.
5. Manipulation under anaesthetics.
6. Open/Arthroscopic capsular release.
Non-Operative Treatment:
Studies on non-operative treatments for frozen shoulder have shown that physiotherapy improves range of movement but not necessarily pain relief. Steroid injections have a benefit for short-term pain relief only but no long-term pain relief (Ryan's Rheumatology 2005, Haslan and Celiker Rheumatol int 2001, Bulgnann Ragum Dis 1984).
Surgery:
Early surgery has been shown to be of significant benefit for a faster recovery of pain, quicker recovery of function and earlier return to work (Hill Orthopaedics 1988, Doddonhoff JSES 2000). Arthroscopic capsular release has been shown to avoid the complications of manipulation under anaesthetic. It has the advantage of being able to identify any other associated pathologies. Numerous studies have demonstrated the benefit of capsular release, although no study that we are aware of randomises patients directly comparing MUA to arthroscopic release. Our own study of 48 patients undergoing capsular release followed for 18 months, demonstrated significant improvement by 5 months postoperatively for resistant frozen shoulders. The Constant score improved from 14 preoperatively to 66 postoperatively, with 80% satisfaction. Range of movement improved significantly by 5 months (Boutros, Snow and Funk 2006).
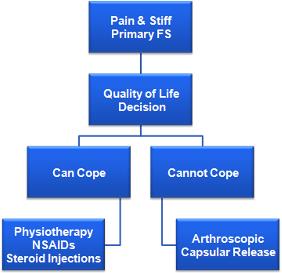
Treatment Algorhythm.
Treatment algorhythm is based on the ability of patients to cope and the significance to cope with the pain and stiffness during the stages of frozen shoulder. This is summarised below:
Conclusion:
Primary idiopathic frozen shoulder is an extremely disabling condition, which does pass through a typical 3 stage progression. However, full recovery at the conclusion of the 3 phases is not common. Early surgical intervention has significant benefits for those patients that are unable to cope with non-operative treatment.


