Injections for Rotator Cuff Disease
WHAT WHERE AND WHY
Lenard Funk
Presented at EUSSER London 2012
In order to achieve good results it is imperative to get the ‘who, where, when, why and what’ decision making correct to ensure a successful outcome for your patient. With regards to rotator cuff disease injections are performed either in the presence of rotator cuff impingement or where there is a partial or full thickness rotator cuff tear.
With regards to subacromial impingement the pathology involves a rotator cuff dysfunction resulting in a mechanical impingement and compression of the subacromial bursa between the rotator cuff and the acromion and coracocromial ligament. This results in subacromial bursitis, subsequent pain, further rotator cuff dysfunction and further impingement. This leads to the vicious cycle of an impingement syndrome.

When to inject
The decision when to perform subacromial injection is based on a failure to progress with the rotator cuff rehabilitation due to the pain. The pain prevents the physiotherapist and the patient from being able to perform the exercises required to rehabilitate and stabilise the rotator cuff. Patients in this group usually have significant night pain with an inability to lie on their shoulders and restricted activities in lifting their arm above shoulder level, typical mid-arc impingement pain. Passive impingement tests are all positive, these being the Neer’s sign, Hawkins’ and modified Hawkins’ impingement tests and the Copeland’s impingement test. Scapular assisted testing should be negative as should scapular corrective testing, i.e. the mechanical impingement features are not correctible by altering the mechanical mal-alignment.
The aims of a subacromial bursal injection are to reduce the bursal inflammation achieving pain relief and allowing the rehabilitation to progress. The rehabilitation involves recentering the shoulder, rotator cuff strengthening, postural and scapula correction.
How to inject
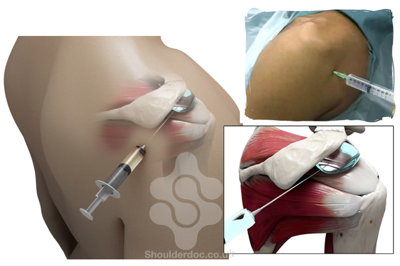
Injections are most often performed without imaging guidance (blind). My personal preference is via the posterior approach but it can be performed via the lateral or anterior approaches depending on ones experience and training. The posterior approach involves an injection 1cm below the posterolateral acromion with a long 18 gauge needle extending into the bursa. The subacromial bursa lies anteriorly and the needle should extend into the bursa. The injectate should proceed without any resistive pressure and often an expansion of fluid can be seen anterolaterally consistent with inflation of the bursa. I would normally inject 10-15ml volume.
Blind subacromial injection via the posterior approach
Blind injections however are not a 100% accurate and studies have shown that the accuracy is 76% via the posterior approach, 69% via anteromedial approaches (Henkus, 2006). There was approximately a 66% correlation between the injector’s confidence in being in the subacromial bursa and accuracy as confirmed on post-injection MRI scanning. An accurate injection was associated with good pain reduction with VAS (visual analogue score) and Constant score returning to pre-injection level at six weeks in all patients. In 51% of cases the rotator cuff was injected in addition to injecting the bursa. There are a number of studies looking at the accuracy of ultrasound and blind injections.
Narido et al. 2004 performed a randomised trial of 41 patients between blind and ultrasound-guided injections. They showed a significant improvement of the ultrasound-guided injections compared to the blind injections at five weeks. Chen et al. performed a very similar study. This involved 40 patients. Interestingly they found no significant difference in pain relief between the guided and blind groups but found an improvement in the abduction range in the ultrasound group compared to the blind group. A number of other studies have also suggested improved accuracy and results with ultrasound-guided injections, however the evidence is not overwhelming or irrefutable.
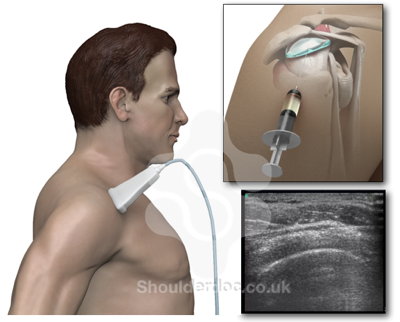
The ultrasound-guided injection is performed in a slightly different way. The injection is actually sub-deltoid rather than subacromial. In performing the technique the bursa is slightly compressed between the rotator cuff and deltoid reducing the access, therefore good visualisation is essential to ensure one is adequately in the bursa. As the fluid is injected it is seen to run within the subacromial bursa rather than dissoluting over a wider area (extra-bursal).
Ultrasound guided subacromial bursa injection
Blind or Guided?
So now we have seen the pros and cons of the blind or guided procedure, in practice how does this translate. My personal approach is to perform a blind injection in the vast majority of impingement and bursitis cases. The technique is quick and simple and reproducible with good training. As shown above it works in over 70% of cases. The guided technique has a role in either the failed initial injection, diagnostically in patients with slightly less specific impingement features. In patients who have undergone previous subacromial surgery a guided injection is probably better.
I personally prefer doing them myself as I can clinically assess the patients immediately after the injection as part of a Neer’s test and also then I know whether I have achieved a good bursal injection or not.
What to inject
Corticosteroids
Traditionally corticosteroids have been the substance of choice. These are both cheap and have been used for many years. They are a very strong anti-inflammatories. The efficacy of corticosteroids is short (Buchbinder, Cochrane review, 2005). The efficacy of corticosteroids ranges from approximately 50-84% in RCT clinical studies (Plafki, 2000; Blair, 1996). In terms of the dosage De Young (1998) showed that 40mg Triamcinolone had a better affect than 10mg. There has been shown to be no difference or benefit comparing 40mg to 80mg.
However there are problems with corticosteroids. They have been shown to be proteolytic and inhibit collagen formation in both cartilage and tendon. There is a high incidence of post-injection pain for approximately twenty four hours in many cases and the efficacy has been shown to be only of short term benefit. Corticosteroids are associated with tendon weakening and rupture, transient hypoglycaemia, lipoatrophy and fat necrosis. Our biggest concern in injecting around the rotator cuff is the risk of additional tendon rupture and tendon damage.
How many injections
With regards to the number and frequency of steroid injections there is no good evidence for this. Three has traditionally become to be the magic number. Whether this is three per year or a course of three or three in a lifetime is not at all clear and left to individual clinicians judgement and experience.
Hyaluronans
Essentially with any treatment our adage in medicine is to first do no harm. Therefore there are other substances that we could inject that would be safer to the rotator cuff tendons. One of the substances that has shown to have a kinder effect on the rotator cuff is Hyaluronans. Hyaluronans are a normal substance within synovial fluid making up the meshwork of the synovial fluid with viscoelastic properties. Hyaluronans act as a joint lubricant. However this is not the effect that is required for these injections. They have been shown to have an anti-inflammatory effect - both mechanical as well as biochemical in inhibiting phagocytosis, reducing levels of prostaglandins, interleukin 1, free radicals and cyclic AMP. They also tend to have a barrier affect coating the pain receptors on the synovial surfaces forming a protective barrier. They have also been shown to stimulate endogenous Hyaluronan production and therefore having a longer period of activity than corticosteroids.
Shibata et al. (JBJSA, 1999) performed a randomised control trial of steroids versus Hyaluronan in patients with rotator cuff tears prior to surgicalintervention. Cuff biopsies were then taken. They found the patients were treated with Hyaluronan, had denser collagen fibres compared to the corticosteroid group. They stated there was a link between the number of steroid injections and the outcome of surgery with a higher failure rate in rotator cuff repairs in those patients treated with a higher number of corticosteroid injections.
Blain in 2008 performed a randomised controlled trial. The study involved 660 patients in Hyaluronan three or five injections versus placebo. They showed a significant improvement in pain scores in the Hyaluronan’s compared to placebo with no difference between three or five injections.
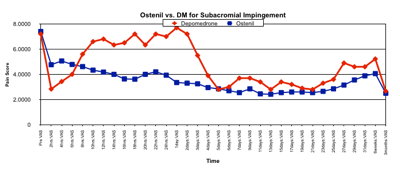
Funk et al. also performed a small randomised study of Ostenil Hyaluronans versus Depo-Medrone for subacromial impingement. We found at three months there was no difference in the pain score between the two groups. The only difference was in the first twenty-four hours after injection where there was a better reduction in pain in the Hyaluronan group compared to the Depo-Medrone group.
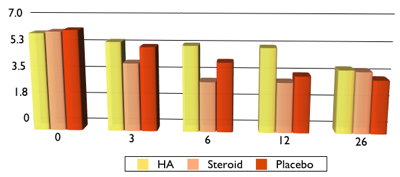
Pennig (JBJSA, 2012) performed a very similar study , randomising into three groups - Hyaluronan, corticosteroids and a placebo. 159 Patients were recruited, with a 26 week follow up. They found at three weeks there was a better effect with the corticosteroid group compared to the Hyaluronan and placebo but by 26 weeks there was no difference between Hyaluronan, placebo or corticosteroids.
My approach
So why do we inject corticosteroid and Hyaluronan and in which circumstances? My personal preference and experience is to use Tramcinolone for the vast majority of cases. These include impingement cases and elderly patients with rotator cuff tears where we are probably not considering repair of the rotator cuff but in younger more active patients where we may be considering a rotator cuff repair but the patient does not want to or is not able to undergo a repair, Hyaluronans are preferred.
Platelet Rich Plasma (PRP)
Another substance that has received a lot of press over recent years is platelet rich plasma. We know platelets are involved with tissue healing, with a high concentration of growth factors.
Platelet Rich Plasma (PRP) is a high concentrate of platelets taken from a patient. Many products also include the white blood cells. These have the ability to manage the immune system and reduce pain. The process involves withdrawing blood from the patient and centrifuging the platelets into a concentrate. The platelets are then activated and injected into the area of injury.
There is a lot of laboratory evidence for the benefits of PRP but there is little good clinical evidence for the rotator cuff, with only small, low-powered studies. There is some clinical evidence for tendonopathies, particularly tennis elbow and Achilles tendon. However these studies are small in number as well as in sample sizes. There is only level 4 evidence on partial or interstitial rotator cuff tears or cuff tendonopathy, these being small case series.
My personal interest is in athletes with partial thickness or joint sided rotator cuff tears. These patients often have pain but not severe enough to undergo surgery, but severe enough to limit their activities and sport. Surgery is associated with a long period of rehabilitation and return to sport, along with the risks of surgical intervention.
Partial thickness rotator cuff tear in the overhead athlete:
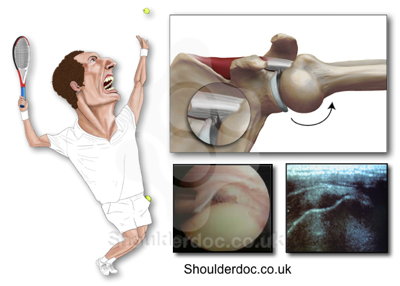
Intratendinous defect in the athlete:

In this very select group of patients PRP may have a benefit in allowing healing of the interstitial and partial tear. In these cases I perform an ultrasound guided PRP injection into the interstitial or partial thickness cuff tear.
Ultrasound Guided PRP injection into the intratendinous defect:

Summary
In summary in patients with subacromial impingement are severe enough to affect their sleep, activities and resistant to rehabilitation, I would inject 40mg Kenalog in 10-15ml of Bupivocaine using a blind technique. In those that have had failed blind injections or I need more diagnostic accuracy or previous bursal surgery I perform an ultrasound guided subacromial injection.

In patients with a rotator cuff tear a Kenalog injection would be my treatment of choice for those patients who are elderly and most likely not going to be proceeding with a rotator cuff repair. In those patients where we would be considering a rotator cuff repair, particularly the younger and more active patients, with traumatic tears, I perform an Ostenil Hyaluronan injection. For interstitial tears in athletes or partial thickness tears in athletes I would consider a PRP injection under ultrasound guidance.



