Arthroscopic Weaver-Dunn
L Funk & M Snow, 2005
The procedure is performed under general anaesthetic in association with regional anaesthesia. We prefer to place the patient in the beach-chair position; the head is slightly deviated towards the contra lateral side. The shoulder should be completely free for full rotation with the anterior and posterior shoulder girdle exposed.
Prior to beginning surgery it is imperative to determine that it is possible to reduce the dislocation. This is done by pushing up the arm while the clavicle is pushed down. Care must be taken during draping to allow access from the top of the shoulder girdle to the base of the neck.
There are 5 portals utilised during the procedure.
1. Standard posterior – 2cm inferior and medial to posterolateral corner of acromion
2. Standard Lateral – 4cm inferior to lateral acromion
3. Anterolateral – 2cm anterior and lateral to the anterolateral corner of the acromion.
3a. Posterolateral – approximately 2cm lateral to the Posterolateral corner of the
acromion.
4. Anterior to ACJ
5. Posterior to ACJ
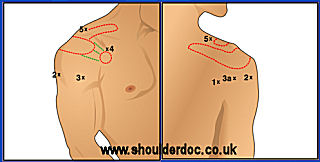

Except for the standard posterior portal all portals are made using an “outside in” technique.
After routine inspection of the glenohumeral joint the bursa is entered and inspected with the camera place through portal 1.
Using a 90 degree hook electrode (Mitek, Depuy) through portal 3 the coracoacromial ligament is identified and mobilised along its lateral border from the acromion to the coracoid. 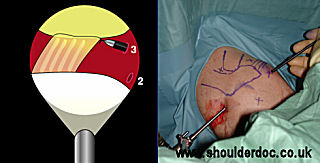
Via portal 4 the medial border of the ligament is mobilised. 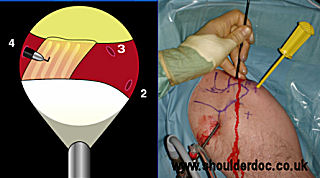
A corkscrew Spectrum suture passer (Conmed-Linvatec) is loaded with No.1 PDS and used to place a suture through the acromial end of the CA ligament via portal 2 or 3. This process is repeated to create a whipstitch. A second PDS is placed in the same manner to achieve a firm grasp of the CA ligament. The CA ligament is then peeled off from its insertion on the acromion using the hook electrode. It would be possible, if preferred, to undertake this step using a small osteotome thus removing a small amount of bone with the ligament.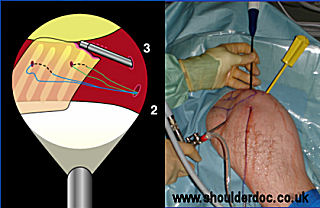

Mobilised CA Ligament: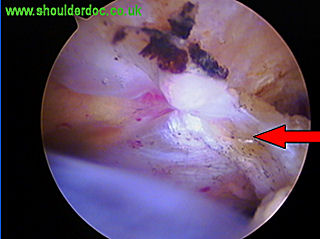
The dislocated ACJ is then identified. The assistant reduces the clavicle, and the lateral end is excised through portal 4 and 5 according to the surgeons preferred technique. If the clavicle is not fully reducible then further debridement may mobilise it enough to allow excision. If after debridement it is not possible to excise the clavicle arthroscopically, this step can be done via a minimal open technique after extending portal 4 or 5. 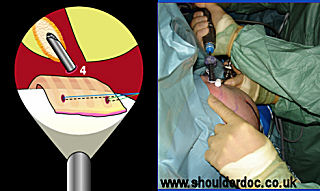
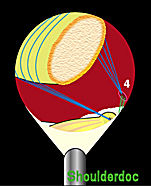
An LPS VAPR radiofrequency probe (Mitek, DePuy) is used through portal 3 to identify the coracoid process. The superior border needs to be clearly visible, without detaching the coracoid insertion of the CA ligament. This is done by keeping the probe medial to the insertion. The scope can be placed in portal 3 to enable improved visualisation of the coracoid. 
A long 2.4mm drill (Mitek, DePuy) via portal 4 is then used to place 2 pilot holes in the coracoid (1 anterior and 1 posterior). A double thread anchor loaded with a strong No. 2 suture is then inserted into each drill hole via portal 4. 
A suture manipulator is placed through portal 5 and all 4 sutures from the posterior anchor are retrieved. These sutures are retrieved subcutaneously from portal 4, over the clavicle, using the same suture manipulator. The 4 sutures from the anterior anchor are then retrieved and pull out through portal 5. The assistant then reduces the clavicle once more and the sutures are tied, using a large hole knot pusher (Mitek, DePuy). The reduction of the ACJ can be visualised arthroscopically, thus complete reduction can be achieved before tying the sutures. 
Once the clavicle is reduced, the transfer of the CA ligament can be achieved. An anchor is loaded onto one of the PDS suture limbs previously placed in the CA ligament. With the camera still placed through portal 3 the anchor is inserted into the under surface if the distal clavicle. The process is then repeated with the second suture in the CA ligament. The sutures are then tied individually, thus transferring the CA ligament to the distal clavicle. If it is noted at this point the CA ligament appears to be short, the anterior insertion on the coracoid can be released safely under direct vision to create more length.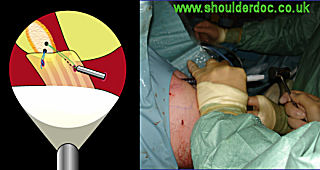
POSTOPERATIVE CARE
Postoperatively the arm is immobilised in a sling for 6 weeks. During this time the patients are allowed to perform pendulum and active assisted exercises. After this time, the patients can use his arm for most everyday living activities. Heavy lifting and resisting exercises are prohibited for a further 6 weeks. After recovery of full range of motion of the shoulder, muscular rehabilitation and sports-specific rehabilitation patients are allowed to return to contact sports. This is usually at three months post-operatively.
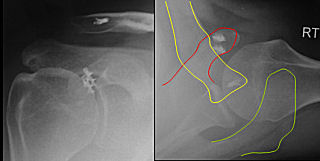
Pre- and Post-operative x-rays: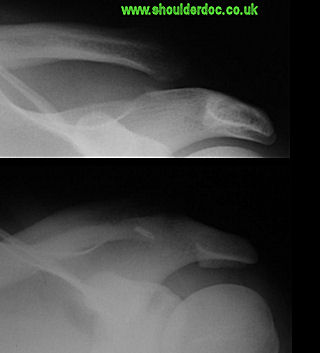
Post-operative wounds:

Return to rugby at 3 months:


