Hemiarthroplasty for Fracture (Neer Type)
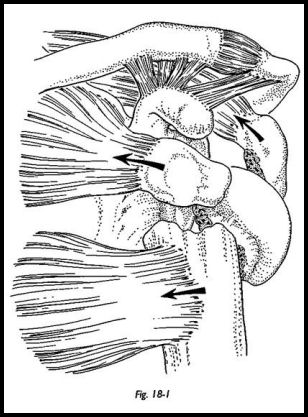
Neer developed a four-segment classification system, -which remains the standard for the evaluation and treatment of these injuries. A displaced fragment is defined as one with displacement of more than 1 cm or angulation of more than 45 degrees (Fig. 18-1). The radiographs must be adequate to identify the precise location of the lesser tuberosity, greater tuberosity, humeral shaft, and humeral head segments. These can usually be seen on three standard views: anteroposterior, lateral scapular, and axillary view, the so-called trauma series. If there is any doubt as to the localization of these fragments—there sometimes can be difficulty in elderly osteoporotic or the fat patients—then computed tomography (CT) scan can be extremely helpful. It is assumed that a humeral head devoid of muscle attachment (i.e. through the tuberosities) is also devoid of blood supply and hence has a high chance of developing avascular necrosis.
Many methods of internal fixation of proximal humeral fractures have been described, but the above techniques are usually best used when residual unfractured tuberosity or soft tissue are adequate to enable the surgeon to determine that the remaining blood supply to the humeral head is adequate. The articular surface of the humeral head may be involved in the fracture anatomy (i.e., head split fracture) or may be separated from its blood supply as in a four-part fracture. Occasionally, the bone may be of such poor quality that rigid internal fixation is impossible, and reconstruction of the proximal fracture may be better done around a rigid prosthetic scaffold. In the younger patient, one must always try to err on the side of caution; if there appears to be any chance the head has an adequate blood supply, then it must be given the benefit of the doubt, and internal fixation and reconstruction of the proximal humerus should be made without prosthetic replacement. However, if there is reasonable doubt as to viability of the head, then primary prosthetic fixation will give more reliable results in terms of function and pain relief. Another factor to be considered is that the best operation is the first one. If the first operation is done for reconstruction and the humeral head then undergoes avascular necrosis, a second operation is required to do prosthetic replacement. The results of the second operation are never as good as the first.
Indications
Four-Part Fracture and Fracture Dislocations
The primary indications for prosthetic replacement are four-part fractures and fracture dislocations. The tuberosities with their attached muscles are displaced from the shaft and the head fragment. In addition, the shaft fragment is displaced by the pull of pectoralis major. Accurate reduction and fixation of these fragments are difficult, and the reported late incidence of avascular necrosis is 80 to 90 percent.1 Concern does exist over treating the younger patient with primary prosthetic arthroplasty, but the results appear to be better with prosthetic replacement than with internal fixation inique.
Head Split Fractures
Head split fractures with a significant step in the articular surface causing joint incongruity 'with associated poor-quality bone stock for fixation can make operative reduction and fixation of the articular fragments impractical. Particularly when these fractures are associated with a crushing element to the humeral head, a prosthetic replacement may be a better option.
Large Hatchet Deformity (Hill-Sachs Lesion)
Hill-Sachs lesion -with traumatic anterior glenohumeral dislocation may be associated with significant impaction fracture of the humeral head on the anterior margin of the glenoid if more than 50 percent of the humeral head is involved. Under these circumstances, gaining stability of the joint may be difficult without prosthetic humeral head replacement.
Three-Part Fracture Displacements
In patients with three-part fracture displacements, one tuberosity remains attached to the humeral head fragment. The soft tissue vascular attachment may be adequate to maintain viability of the humeral head. However, this fracture pattern is commonly seen in the elderly, the blood supply may not be adequate, and avascular necrosis can occur. Also, the bone stock may be poor, and difficulty may be experienced in achieving rigid enough internal fixation to allow for early mobilization. A better fixation and thereby earlier mobilization, may be achieved by prosthetic replacement of the humeral head.
Preoperative Investigation
Younger patients who sustain four-part fracture dislocation have often sustained severe and multiple trauma. Their general condition may not allow operation until other more life-threatening injuries have been treated. A neurovascular injury must be excluded before surgery. An accurate assessment of the fracture pattern must be achieved before surgery by trauma series radiographs; if this is not adequate, a CT scan may be helpful.
Position of Patient
The standard beach chair position is used. The patient is under general anaesthesia with a sandbag under the affected shoulder and an arm board attached to the table supporting the arm.
Technique
The extended anterior deltopectoral approach is used.
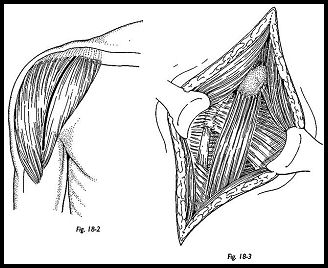
The deltoid and pectoral muscles are retracted, and the clavipectoral fascia is incised up to the level of the coroacromial ligament. Sometimes the fascia has been disrupted by the fracture fragment (Fig. 18-2). The coracoid muscles need not be detached but just retracted medially (Fig. 18-3). If access is difficult, a small portion of the deltoid insertion may be detached from the shaft of the humerus or the origin from the clavicle, but it must be reattached at the end of the procedure. A retractor is then placed under the deltoid, superficial to the cuff muscles, and the fractures are palpated. The biceps tendon is a very useful landmark, because it usually remains intact and is a guide to the interval between subscapularis and supraspinatus, that is, a delineation of the greater and lesser tuberosities. Tuberosity segments may well be comminuted and retracted but must be localized and secured with stay sutures. The subscapularis is elevated with the lesser tuberosity, the joint is explored, and the head fragment is removed. This can sometimes be difficult in fractures associated with a posterior dislocation because the head fragment may well be locked posteroinferiorly. Loose fragments are removed from the joint once the tuberosities have been retracted.
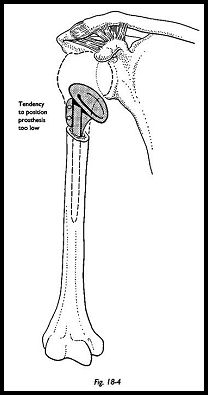
The humeral head is retained as a possible source of bone graft. Once the humeral head has been removed, the shaft segment is presented into the wound by extension of the arm over the edge of the short arm board on the side of the operating table. If any bone fragments are removed, they are carefully kept so that the length of the humeral shaft can be estimated. It is of extreme importance to place the center of the prosthetic humeral head at the level of the center of the anatomic humeral head (Fig. 18-4). The most common mistake is to seat the prosthesis too distally using the remaining bone as a seat for the neck of the prosthesis. This will have the effect of shortening the humeral shaft and relatively lengthening the surrounding musculature. It will hence be unstable and will never regain a reasonable range of motion.
The humeral shaft is then prepared using the graduated T-handle reamers. The stem size is then selected, being the largest that the humeral shaft will accommodate. Assessment of head size is made using the retrieved fractured humeral head as a template. A trial reduction is then made, and the tuberosities with their stay sutures are brought round the neck of the prosthesis to assess ease of reduction and tension of the rotator cuff. These may be temporarily fixed with the towel clip around the fin of the implant. The two most essential steps in the procedure are establishing the correct tension of the rotator cuff and the correct height of the prosthesis within the humeral shaft. In general terms, the largest head that allows for closure of the cuff and tuberosities around the fin is the one selected.
Angle of Retroversion
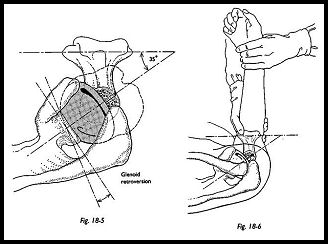
The correct angle of retroversion is approximately 35 degrees, but this may be estimated in one of several ways. The prosthesis is inserted in the shaft, and with the elbow flexed to a right angle, the forearm is used as a goniometer (Fig. 18-5). If the prosthesis is first placed at 90 degrees to the forearm and then the forearm is externally rotated in relation to the prosthesis 35 degrees, the correct angle of retroversion will be achieved (Fig. 18-6). This is then checked by looking down the humeral shaft from above. If the prosthesis is correctly placed, this should leave the fin of the prosthesis pointing toward the posterior lip of the biceps groove. Finally, a trial reduction is made, and the range of movements is assessed.
Fixation of Prosthesis
Cement is invariably used, and only rarely can a press fit be relied on. It is vital that the prosthesis is set at the correct level in the shaft, and it is unlikely that this correct level will exactly correspond to the level of the tightest press fit. The humeral shaft is prepared in the usual way with pulsed lavage, the shaft is dried, and at least two proximal drill holes are made with sutures passed through ready to attach to the tuberosities. The sutures are left in place while the cement is inserted down the shaft. The prosthesis is then inserted, and the angle of retroversion is checked. The tuberosities are Hghtly pulled round the humeral neck and placed in the anatomic position so that the height of the prosthesis can be judged. The correct height is indicated as follows:
- The tuberosities fit like a jigsaw puzzle with no bone loss.
- The tension in the biceps tendon is adequate, and the tension in the rotator cuff anatomic.
- f the arm is pulled distally, the humeral head should not be able to be subluxed more than one third in relation to the glenoid.
If all these are correct, then the cement is allowed to set.
Reconstruction of Tuberosities
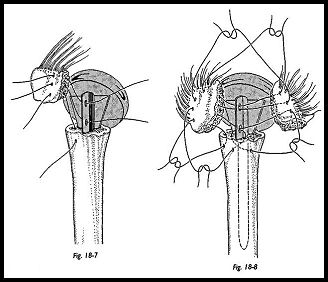
If late displacement of tuberosities is to be prevented, it is essential that they heal both to the humeral shaft and to one another. Some nibbling of the tuberosities may be required so that they fit snugly against the prosthetic shaft (Fig. 18-7). Drill holes are made in each of the greater and lesser tuberosities, and a heavy suture is used to secure the tuberosities to one another and to the fin of the prosthesis. The sutures previously-passed through the holes in the humeral shaft are now passed through the inferior hole in the tuberosity and tied such that the tuberosities are held down to the shaft and to each other (Fig. 18-8).
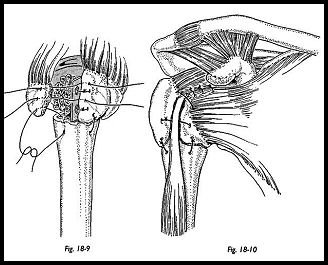
When the sutures have been tied to the fin of the prosthesis, bone graft from the humeral head is packed underneath the tuberosity between the greater tuberosity and the humeral shaft before securing the sutures (Fig. 18-9). The rotator interval between the supraspinatus tendon and subscapularis is then closed with suture, completing the tuberosity and cuff repair around the prosthesis (Fig. 18-10). At this stage, the whole reconstruction must be solid enough to allow early mobilization with confidence.
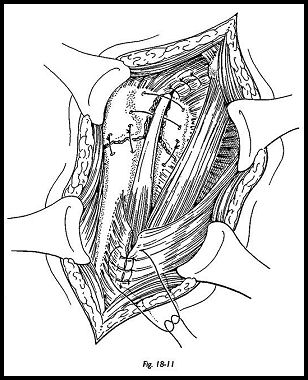
Anterior acromioplasry should be considered if there are any degenerative changes on the undersurface of the acromion, or if it is thought that impingement may be a problem (Fig. 18-11). Finally, suction drainage is placed below the deltoid muscle, the wound is closed, and a sling is applied.
Postoperative Management
At the end of operative procedure, the surgeon should make a note of the range of movements that the shoulder can easily achieve without putting obvious strain on the repaired tuberosities. The rehabilitation program must depend on several factors. The degree of comminution of the tuberosities and the quality of bone available for repair depend on the quality of fixation that can be achieved. In the end, a good result depends on fracture healing—both tuberosities uniting to each other and also to the humeral shaft. Mobilizing, however, cannot wait until fracture union; otherwise, irreversible stiffness will occur. To avoid disrupting the repair, muscle strengthening begin only when bony union has occurred. With these factors in mind, the surgeon must map out in the operative notes the postoperative rehabilitation plan. Assuming secure fixation of tuberosities and soft tissues have been achieved, postoperative management may proceed as follows:
Day 1. Active and passive range of motion exercises is begun for the elbow, wrist, and hand and passive forward flexion-extension in the scapula plane for the shoulder. This must be within comfort limits initially and certainly within the limits defined at surgery.
Day 5. Passive abduction and internal rotation are begun with the patient supine. Pendulum exercises can be started at this stage.
Day 10. Assisted forward flexion is begun using pulleys with the unoperated arm to raise and lower the operated arm.
Day 15. With the patient lying supine, passive external rotation is begun using a walking stick with both elbows tucked in at the side with the unoperated arm pushing the operated arm into external rotation.
Day 21. A static anterior deltoid muscle exercise is begun. No external or internal rotation strengthening exercises can be initiated until the tuberosities are healed.
Weeks 6 to 8. Isometric muscle strengthening exercises are begun for external and internal rotation of the humerus. Forward flexion, stretching, and external—internal rotation stretching are continued with the patient supine.
Week 10. Resistive exercises for deltoid and resisted external-internal rotation exercises are begun using Theraband graduated elastics for resistance. Patients are told that movements will improve for 1 year to 18 months following surgery and that they should continue a stretching program during this time.
After 3 months. Patients are actively encouraged to passively hang, that is, to reach up and push their arm up to a high shelf or door frame, and then drop the body down, passively stretching the shoulder forward and upward.
Results
Hemiarthroplasty for fracture is an operation that is very operator dependent. Experience is required to judge positioning and tensioning of soft tissues at the time of surgery and to gain fixation of bone and soft tissues strong enough to allow a rigorous postoperational rehabilitation program. Prosthetic replacement can give satisfactory pain relief, but the range of motion can be variable. The most satisfactory results are in those patients without any complications. If problems with rotator cuff, displacement of tuberosities, and poor rehabilitation can be avoided, the range of motion in general is quite acceptable.3 A near-normal range of motion can be achieved, but strength depends on the adequacy of the soft tissues, the surgical technique, and the adequacy of postoperative rehabilitation.
Problems -with osteoporotic bone, tuberosity displacement, late rotator cuff problems, and inadequate rehabilitation can limit the functional result. However, with attention to the surgical details, secure fixation of the tuberosities, and an individualized rehabilitation program, this appears to be the treatment of choice for four-part fractures, giving the best results for restoring motion, function, and strength.
References
- Neer CS: Displaced proximal humeral fractures. Part II. Treatment of three and four part displacement. J Bone Joint Surg [Am] 52:1090-1103, 1970
- Stableforth PG: Four part fracture of the neck of the humerus. J Bone Joint Surg Br 66:104-8, 1984
- Cofield RH: Commuted fracture of the proximal humerus. Clin Orthop 230:49-57, 1988
Suggested Readings
Green A, Lloyd-Barnard W, Limbird RS: Humeral head replacement for acute four part proximal humerus fractures. J Shoulder Elbow Surg 2:249-54, 1993
Tanner MW, Cofield, RH: Prosthetic arthroplasty for fractures and fracture dislocations of the proximal humerus. Clin Orthop 179:116-28, 1983


