AC Joint Disloc. Management
Management of ACJ Dislocations
The evidence in 2007
From: Augustus D. Mazzocca, Robert A. Arciero and James Bicos. Evaluation and Treatment of Acromioclavicular Joint Injuries. Am. J. Sports Med. 2007; 35; 316
The main goals of treatment, whether surgical or nonsurgical, are to achieve a pain-free shoulder with full rangeof motion, normal strength, and no limitations in activities. The demands on the shoulder will differ from patient to patient, and these demands should be taken into account during the initial evaluation.
Type I and II:
Most types I and II AC joint separations are treated nonsurgically. Only 27% of conservatively treated types I and II AC joint separations may require further surgery at 26 months after injury [Mouhsine et al].


Type III:
Type III injuries are usually evaluated on a case-by-case basis, taking into account hand dominance, occupation, heavy labor, position/sport requirements, scapulothoracic dysfunction, and the risk for reinjury.
Evidence supporting nonoperative treatment of type III AC dislocations has been provided by a meta-analysis.121 In a review of 1172 patients, 88% who were operatively treated and 87% who were nonoperatively treated had satisfactory outcomes. Complications included the need for further surgery (59% operative versus 6% nonoperative), infection (6% vs 1%), and deformity (3% vs 37%). Pain and range of motion were not significantly affected. The authors did not recommend surgery for type III AC joint injuries. Another study showed that non-operative treatment leads to a 20% rate of suboptimal outcome and 17% decrease in bench press strength at one year, but 80% of people do not feel that it affects them[Schlegel et al]. Larson and Hede prospectively compared nonoperative and operative treatment with similar rates of persistent symptoms (8% in the operative group vs 10% in the nonoperative group).

Type IV, V and VI:
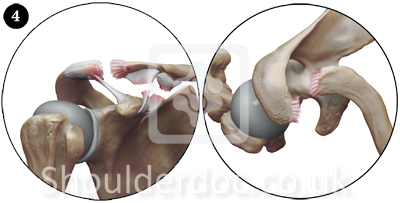
Complete AC joint injuries (types IV, V, and VI) are usually treated surgically because of the significant morbidity associated with persistently dislocated joints and severe soft tissue disruption. The shoulder manifests as a severe droop, secondary to downward displacement of the scapula and humerus due to loss of the clavicular strut. The weight of the arm and the geometry of the chest wall cause an anterior-inferior translation of the scapula around the thorax, referred to as the third translation of the scapula.

Surgical Treatment:
Despite the common occurrence of AC joint separation and the extensive experience with surgery in the treatment of these injuries, only recently have investigators evaluated the biomechanical properties and performance of various augmentation and reconstructive procedures.
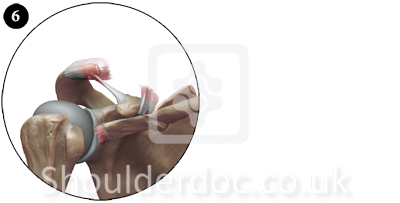
The coracoacromial ligament as a graft source transferred to the distal clavicle represents only 20% of the ultimate load of the intact coracoclavicular ligament complex. Motamedi et al evaluated the biomechanics of the coracoclavicular ligament complex and augmentations used in repair and reconstruction. Augmentations around or through the clavicle improved load to failure and stiffness of the reconstructions. Clayer et al found that a PDS coracoclavicular sling did not maintain reduction, but good results were obtained in
6 patients. Gohring et al and Pfahler et al separately compared PDS cerclage with other techniques. Gohring et al compared the surgical treatment of 64 complete AC joint dislocations with 3 techniques: tension band, Wolter hook-plate, or PDS cord (braided). Early postoperative complications occurred in 43% of patients treated by tension band, 58% of those treated by hook-plate, and 17% of those treated by PDS cord. Acromioclavicular joint instability at an average 35-month follow-up was seen in 32% of patients with a tension band, 50% with the plate, and 24% with the PDS cord. The authors recommended limiting surgery to younger, athletic patients. Loss of reduction of the AC joint is not uncommon. The weight of the arm and scapula places tremendous static forces on the coracoclavicular reconstruction.
Based on these findings and other current research we currently use the LARS Ligament Technique, which does not rely on the coracoacromial ligament and reconstructs the coracoclavicular ligament mechanics.
Also see:
- AC Joint dislocations - Classification & Natural History
- Decision making: operative versus nonoperative treatment of ACJ injuries.
- Other News & Research on ACJ


