Tumors in the region of the subacromial bursa
CHAPTER XIV
ANY reference to skin lesions over the region of the shoulder will be omitted, although it would be appropriate to mention them if I knew of any particular types which might be confused with a bursal lesion or which were especially common in this region, or of any ordinary tumor of the skin which had peculiar characteristics when located on the shoulder. The shoulder may be attacked by skin lesions of any form, the number of which is not as great as the number of the names applied to them. It would be a boon to the general practitioner if the names for lesions of the skin could be codified on the basis of clinical entities, as has been done for bone sarcomas. We should find that the number of skin diseases of importance as true clinical entities would be few in number, compared to the total of their complex mystifying names. I will merely mention that Herpes Zoster ("Shingles") may affect the nerves on the dorsum of the shoulder and be the cause of obscure pain.
Lipomas of the subcutaneous tissue do have a peculiar relation to this region, for this form of tumor seems to occur with great frequency about the shoulders. They are of actual importance in diagnosis in relation to lesions of the bursa, because not infrequently the pain caused by a shoulder injury is referred to a lipoma which may have been there unnoticed for some years. The accident perhaps served to call the patient's attention to it in his search for the cause of the local pain. I noted the presence of lipomas in a little over one per cent of my cases. I have several times seen one on the tip of the shoulder exactly over the subacromial bursa, so that its external appearance simulated a swelling due to distention of the bursa itself. Usually these tumors are posterior rather than anterior, but they may overlie the acromion. They may assume great size, but are usually small, varying in size about as much as does an oyster, and they are often of a similar shape. Owing to the tough skin on the dorsum of the shoulder, they remain quite flattened, and if an attempt is made to remove them, they do not shell out as easily as do similar tumors in other parts of the body. Several patients were very emphatic in saying that the tumors had not been there before the accident, although of course they probably had been there for a long time. Theoretically, it is possible that a local bruising of the subcutaneous fat might initiate the onset of a lipoma. Personally, I think this is very unlikely; the reader is referred to the discussion of the traumatic origin of bone tumors at the end of this chapter.
.jpg)
FIGURE 67. SIMILARITY OF APPEARANCES OF LIPOMA AND DISTENDED BURSA
a. A lipoma, the situation of which is almost exactly over the subacromial bursa. b shows the shoulder of the patient from whom the X-ray in Figure 44 was made. The greatly distended bursa makes the contour of the shoulder appear swollen, although the swelling is wholly beneath the deltoid.
Fascial tumors are not common about the shoulder except in close relation to the bones, when they would be called periosteal fibromas or fibro-sarcomas, according to the nomenclature of the Registry of Bone Sarcoma. I have the impression, however, that this rare form of tumor is relatively more common about the scapula than about other bones.
The subject of bone tumors in relation to the shoulder joint will be taken up in some detail, partly because I have been interested in the Registry of Bone Sarcoma, and partly because I believe that any surgeon who is studying lesions of the bursa should be prepared to encounter lesions of those structures which are adjacent to it.
Before taking up the diagnosis of the different tumors which occur in the shoulder, let me present some theories which have occurred to me in regard to Bone Tumors in general. The shoulder joint is a region in which all the different forms of bone tumors are found. The bones of the shoulder do not play favorites as regards the different kinds as do many of the other bones. For instance, osteogenic sarcoma very rarely, if ever, affects any of the small bones of the fingers or toes. A tumor of the lower end of the radius is almost always a giant cell tumor. Osteogenic sarcoma seems to have an aversion for the lower end of the tibia. Myeloma prefers a rib, and ribs prefer myelomas. Ewing's sarcomas select the shaft of a bone, while giant cell tumors prefer the epiphyses. A tumor of the shaft of the bone, with a metastasis in the skull, would probably be an instance of Ewing's sarcoma.
I am convinced that the various forms of tumors differ somewhat in detail according to the bone that they attack, and that they, to some extent, mimic the form or characteristics of the part of the bone that they are in. Thus in the future, I believe that it may be possible for a pathologist expert in bone tumors to guess, from the microscopic appearance, not only what bone the tumor is probably in, but what part of that bone. At present there are vague indications that such detailed diagnoses may be made; an instance is a form of giant cell tumor involving the tuberosities of the humerus, which is more common in this region than in any other.
It would seem to me that not only does the character of the tumor vary with the individual bones of the skeleton, but that some forms of tumors have abortive morphologic plans, as do the peculiar growths called "galls" formed on trees and plants, some of which resemble leaves, some flowers, and some bark. For instance, some osteogenic tumors, both benign and malignant, tend to form cartilage on their surfaces and to have bony bases, thus resembling roughly in form the condyles of a joint. Some of the lesions, such as benign osteogenic tumors of the fingers, resemble a twin of the phalanx itself. If in an osteogenic tumor there is a portion bulging into the popliteal space, this portion will generally be composed of cartilage, resembling in shape the big knobs of the joint cartilage. Osteogenic sarcomas, as a whole, resemble a normal callus about a fracture in their fusiform contour, and in their activities, which are always both intra- and extra-cortical. I have come to believe that tumors exhibit an architectural plan (to be sure, a very irregular one), but resembling the same mysterious morphologic design which makes the normal cells form the definite part in which the tumor arises. According to this idea the malignant impulse must be given rather to the plan than to the tissue in which the potentiality of repair lies. The normal repair process knows when its specifications are completed, but the malignant repair process has lost its growth or repair restraint and goes on unchecked, but still vaguely follows the plan of the part of the bone involved.
Analysis of Registered Cases of Tumors of the Shoulder Bones
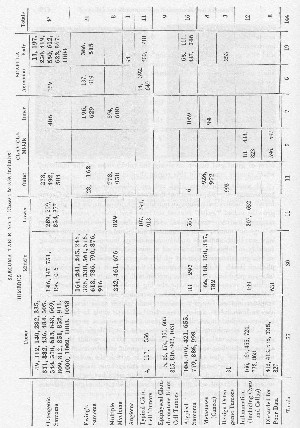
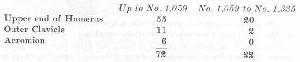
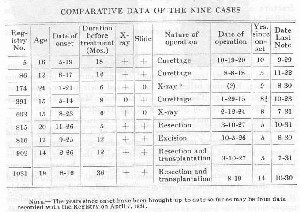
In order to write this chapter advantage has been taken of the opportunity offered by the Registry of Bone Sarcoma, and in the summer of 1930 the following study of the cases registered up to No. 1,059 was made. Table I shows the relative frequency and the sites at which the different forms of bone tumors occur in relation to the shoulder joint as far as may be judged from the evidence of the 144 cases which involved the humerus, clavicle, and scapula. Notice that the figures are the Registry numbers of the cases, except for the marginal ones, which indicate the totals in each lateral or vertical column.
In April, 1932, a second study was made and the mortality, as indicated by the heavy type on the charts, brought up-to-date, and the text revised accordingly. Table II was prepared from the cases registered since the previous study from No. 1,059 to No. 1,335, but was not used in the text because there was nothing found in this second study except confirmatory evidence for some of the observations already made. The chief value of Table II is to indicate in a general way that the relative figures are much the same as in the first study, e.g., in both tables thirteen and one-half per cent of all bone tumors were in the shoulder bones, and osteogenic sarcoma in the head of the humerus is the most common shoulder tumor. However, in Table II there is a notable lack of giant cell tumors. Furthermore, Table II might be of value to any future student of this subject, for it gives him the Registry numbers for ready reference so that he can send for their envelopes for his own study. The cases in Table II are too recent for the results to be of statistical value.
A large proportion, seventy-two of the one hundred and forty-four tumors of the shoulder, lay in relation to the subacromial bursa, for they involved the acromion process, the outer end of the clavicle and the upper end of the humerus. They probably rarely actually invade the bursa. Nevertheless, we must consider them if we are to be prepared to make detailed differential diagnoses of conditions affecting the shoulder. Even after I had studied shoulder conditions for many years, I operated on a patient under the diagnosis of subacromial bursitis, and later found that this had been an unnecessary operation, for although there was a bursitis, the pain had been really due to early metastatic cancer in the upper end of the humerus. At the time of the operation the X-ray showed no evidence of invasion of the bone. Shoulder pain is the first symptom of most tumors of the head of the humerus, and while it is quite true that hitherto no early cases of bone tumors have been diagnosed, there is, nevertheless, hope that in the future we may learn, either by careful X-ray or clinical findings, to discover bone tumors in their infancy. We must keep the question in mind in the case of every painful shoulder. Of the 1,335 tumors in the Registry collection on April 7, 1932, not one can be said to be in an early stage. Some were discovered soon after symptoms began, but the X-ray showed the disease well advanced.
It is sometimes well to stop to consider relative proportions, and as I am a general surgeon who has had among other hobbies the studies of bone sarcoma and of obscure shoulder lesions, the reader may be interested in my comparison of their frequency. Bone sarcoma, though more serious, is not as common as rupture of the supraspinatus tendon in ordinary everyday life. The relative frequency of the two lesions may be contrasted by the fact that Dr. Akerson was able to find lesions of the supraspinatus in thirty-nine of one hundred consecutive shoulders at autopsy, as compared to the fact that the Registry of Bone Sarcoma, sponsored by the American College of Surgeons, whose membership is over 7,000, has in ten years been able to collect records of only 144 cases of tumors in the shoulder bones. To be sure, rupture of the supraspinatus tendon is usually not recognized, while tumors of the bone present such dramatic, pathetic and fatal pictures, that if one case occurs in a hospital, every doctor connected with the institution will probably see and know about that case. The rapid advance, the grotesque appearance, the fatal ending (which is the usual history in bone sarcoma), attract attention, whereas rupture of the supraspinatus never causes death, and is difficult to demonstrate, even when the diagnosis is made. Many surgeons have not yet even heard of it, much less can they diagnose it. I therefore enter as a preliminary statement that I know that this chapter is disproportionate in size to the rest of the book, yet not so disproportionate as is the literature of bone sarcoma to that of the supraspinatus.
Before speaking in detail of bone tumors, let me say something of the Registry, and in order to do this, I should like to present a facsimile of the face of a ten by twelve inch manilla paper envelope which the Registry uses to contain the data of each case. The reading matter on this envelope has been given a great deal of thought, and I beg the reader to take a magnifying glass and to study it in detail. The central, vertical division is apparently the most important, because it contains a list of bone tumors and purports to be a standard classification for common use for surgeons, rontgenologists and pathologists. This has been the working classification for the American literature of this subject for the last decade, but experience shows that it needs improvement. At the bottom of the Registry envelope two sentences occur which are of great significance,.
"It is believed that this list covers all bone tumors which are known to have a natural history distinct enough to justify prognosis or to indicate special treatment. If you believe there are others, please register illustrative cases." This rule should exclude serious discussion of other old or new terms, unless definite data are filed on which the committee may open discussion.
If a patient has a tumor of one of the shoulder bones, it should be one of the tumors on this list, which was agreed on by two committees of pathologists. At that time our ideas of the relative frequency in which these tumors might occur were very vague. As experience comes we find that we have now little use for some of the terms. For instance, we all find fault with "periosteal fibro-sarcoma." I could not point today to a single Registry case which typifies what we meant by this term, nor has any article appeared in the literature of the last decade which presents a study of a group of such tumors. We did mean something by the term, and it still has some value, but most of us would prefer to use parosteal or extra-periosteal fibrosarcoma for one of these rare cases. We meant a tumor which had nothing to do with the bone, which was fibrous, and arose from the outer layer of periosteum, or adjacent fibrous tissue. Experience has shown that such tumors are rare.
In fact, our whole understanding of the term "periosteal," in relation to sarcomas, has gradually changed. For instance, we find that practically every case of osteogenic sarcoma is both "medullary and subperiosteal." Since the term applies to all cases, it is of no special significance. We also made what I consider a mistake, of using the term "periosteal" to qualify a subdivision of osteogenic sarcoma. We thought then that there was a periosteal sarcoma pure and simple, as opposed to a central sarcoma pure and simple. Some of the committee still cling to this idea, but personally I have never yet seen an osteogenic sarcoma which was confined to the periosteum, and was not intracortical as well. They are always, in my experience, both extra- and intra-cortical. To be sure, one sarcoma may have more than nine-tenths of its bulk extracortical, and only one-tenth intracortical, and another may have more than nine-tenths of its bulk intracortical and less than one-tenth extracortical.
Essentially, these two types are the same and have the same prognosis, and are clearly not different clinical entities. It is, therefore, not logical to say that a tumor arose in either situation because the bulk of it is extra- or intra-cortical.
In my opinion, we should also have left the terms sclerosing and telangiectatic in the left-hand column. They are descriptive adjectives, useful for individual instances, but do not define real clinical entities. It was then held that "sclerosing" cases had a little better prognosis and telangiectatic a little worse than the average. Certainly among the shoulder bones this has not been confirmed, for all the sclerosing cases are dead and one very bad telangiectatic case is a five-year cure (Registry No. 156).
The second subdivision of osteogenic sarcoma, "undifferentiated sarcoma," has practically become an unused pigeon-hole, because the cases which we intended to put in that division are now carried under Ewing's sarcoma. Ewing's sarcoma is characterized by absolutely undifferentiated cells which have no intercellular substance. There may be a few undifferentiated sarcomas which are not Ewing's sarcomas, and which we cannot pigeon-hole in any other place, but as a matter of fact, such tumors are extremely rare, if they exist at all. It is an almost useless division. I prefer to carry the few cases under "Atypical Sarcomas."
The subdivisions of inflammatory conditions were not intended so much as actual subdivisions as examples. Of course, other inflammatory conditions of bone might have been included. I think we might have saved ourselves many explanations by stating that callus and cysts are considered as "inflammatory" in the sense of a tissue reaction to trauma. Normal repair following trauma without infection may be considered inflammation. Inflammation does not necessarily mean infection.
Benign giant cell tumor has proved a fairly distinct class, but there are a few cases in the Registry series, the outcome of which suggests the advisability of dropping the adjective benign. Experience shows that we have had to acknowledge in a very small number of cases that our original diagnoses were incorrect, or else to admit that a malignant tumor became superimposed on a benign condition, or to admit that benign giant cell tumors were not always benign. This subject has been discussed by Geschickter and by Simmons recently, and will not be discussed further by me here, especially as no such instances have occurred in the shoulder bones. Later in the chapter reasons will be given for the belief that benign giant cell tumors of the upper end of the humerus have many characteristics which differ from most of the giant cell tumors in other bones.
Our class of angioma was necessary, and the subdivisions were necessary, for we have had a few unquestioned cases of benign cavernous angioma of bone which have a distinct X-ray appearance and a benign course, in spite of the presence of large tumors in two of the cases. On the other hand, the malignant division of angioma is still of doubtful value. I could not pick out a case from the Registry series which would be a typical angio-sarcoma. The type of tumor called Endothelioma by Kolodny would be the nearest that I know of; yet, since this type is so very rare and still doubted by so many pathologists, and since the few cases we have are regarded by some pathologists as perhaps instances of metastasis from cancer, the term angio-sarcoma is of doubtful value, but it cannot be discarded.
The seventh division (Ewing's tumor) should certainly be modified to Ewing's sarcoma, because this type of tumor is malignant, and since we have used the term tumor in benign giant cell tumor instead of sarcoma, to denote that the giant cell type is benign, we certainly should use the term sarcoma with Ewing's name, because his tumors are surely malignant. For the eighth division (Myeloma), I believe we should use the term Multiple Myeloma, because the English and Canadians, following the British custom, have for years used the term myeloma to signify what we know as giant cell tumor. So far as the experience of the Registry goes, myeloma is always multiple, although we have had a few cases where a single tumor appeared to be present for some time before others developed. It is important to emphasize this multiple character of myeloma on account of the differential diagnosis of Ewing's sarcoma. Ewing's sarcoma is certainly sometimes multiple, but the bulk of evidence goes to show that the tumor is usually primary in one bone and that the involvement of other bones is of a metastatic nature. An increasing number of amputation cures proves this. Myeloma, however, seems to arise in different foci in many parts of the body at once. Ewing prefers the term endothelioma for his tumor, but this is confusing, and most pathologists do not admit that it is endothelial. It certainly is quite different from multiple myeloma, although the two are the only round-celled primary bone tumors. We should simply modify these two terms by saying: (7) Ewing's sarcoma. (8) Multiple myeloma. This would indicate that while Ewing has convinced the American pathologists that his sarcoma is a clinical entity, he has not yet convinced them that it is entitled to the name of endothelial myeloma or endothelioma. The above modifications of the Registry Classification are used in the table.
Under Atypical Sarcomas would fall cases which we cannot assign to any one group, yet we have evidence enough to .feel that they are primary sarcomas and not benign conditions or metastases from cancer. So the term is not the same as Miscellaneous, for it implies "surely sarcoma." Under "atypical" might be put such cases as the sarcomas arising in giant cell tumors or in old osteomyelitis, or any malignant tumor with peculiar histology which is not considered to be a metastasis. The few cases of questionable periosteal fibro-sarcoma might be put in this class also, if it seemed advisable.
The group "discarded" means that the case has been so poorly registered and has such poor data that conclusions drawn from it would be of little or no value for the present purpose. Such cases are not valueless entirely; I have several times learned something from cases reported with very incomplete data. In fact, few of our cases do have absolutely complete data, and it must not be understood that the cases in the table are all positively and permanently diagnosed.
Notice that those tumors above the heavy line are primary, malignant tumors of bone—the kinds which we asked surgeons to register. Those below the line we did not and still do not wish to have registered. We asked for registration of cases of sarcoma; the cases below the line were registered because some one thought they were sarcoma. The inference from this is, that the relative frequency of the tumors below the line with those above the line cannot be estimated from this chart. Actually, the occurrence of the kinds listed below the line is probably greater, for many more of the types below the line might have been registered if we had asked for them. On the other hand, I see no reason why we should not estimate the relative frequency of the occurrence of the tumors above the line from this table, or a similar one drawn from all the Registry cases, including the other bones. Possibly some giant cell tumors have not been registered because some surgeons have thought that we did not wish them, since they were not sarcomas. Time has proved the desirability of following up the giant cell tumors, since we have now a number which have proved to be malignant. None of these were in the shoulder bones, however. Perhaps other surgeons may have refrained from registering myelomas because they were not sarcomas. At any rate, I can see no reason for doubting that the proportion of osteogenic sarcomas and Ewing's sarcomas can be obtained from this chart, except that the diagnosis of Ewing's sarcoma can seldom be made from the X-ray alone, while those of osteogenic sarcoma may be. A significant point is brought out by this chart—that Ewing's sarcoma is quite common in all three shoulder bones.
The chart also shows the probable relative proportion of errors in practical diagnosis, since those cases above the line stand to those below the line as 102 to 32. This is an improvement on Greenough's, Simmons', and Harmer's figures in 1921 in reference to the cases at the Massachusetts General and the Huntington Memorial Hospitals. These authors say:
"Perhaps the most surprising fact of the whole study is that out of 148 cases sent in as possible bone sarcoma, only sixty-six could be considered in fact to be cases of malignant new-growth of bony origin; the remaining eighty-two cases proving on more detailed study to be metastatic tumors of bone (twenty-nine cases), sarcoma primary in the soft parts (twenty-eight cases), inflammatory conditions (eleven cases), or tumors of a non-sarcomatous type (fourteen cases)."
I feel very confident that the degree of accuracy of diagnosis in bone tumors throughout America has greatly improved since the Registry was established in 1920. In the last thirty-eight shoulder tumors registered there were only five to be placed below the line.
Among the first 1,058 registered cases, ninety-six involved the humerus, twenty-three the clavicle, and twenty-five the scapula. So we may say that about every tenth bone tumor will involve the humerus, or out of every ten bone tumors, about one or two will involve one of the shoulder bones. When we confine our study to the portions of these bones which lie near the bursa, we find
The writer (Bone Sarcoma; Prevalence in Massachusetts. Bos. Med. 4- Surg. Jour., 1922, Vol. 187, pp. 208-211 and pp. 543-545.) after a postal card canvass of the physicians of Massachusetts, estimated that only one out of every 100,000 of the population at any one time was afflicted with bone sarcoma. This estimate would be decreased to less than one in 1,000,000 if we specify a sarcoma in the neighborhood of the subacromial bursa. In other words, most physicians will see perhaps one such case in a lifetime. Why occupy a whole chapter of this book with discussion of such a rare shoulder condition?
A glance at the chart gives one good reason, for the cases whose deaths have been reported are in heavy type. Obviously some of these tumors are very fatal and others are not, and while at any one date there may be only one fatal case progressing among every million persons, that means at least a hundred fatal cases in the United States. Delay in diagnosis is the most important obstacle to the prevention of this mortality, and the cause of deep regrets for time and money wasted by treatment for erroneous diagnoses of "rheumatism," etc. Bone sarcoma is practically the only fatal lesion which arises in the shoulder. We must learn to recognize it and to cure it. It should be our first thought in the case of a young patient complaining of a dull aching pain; if any thickening of the bone were palpable or the pain persisted more than a week, we should seek help from the X-ray.
The details of this chapter need not be remembered by the average physician if he will only bear in mind his obligation to see that every patient complaining of pain or swelling about the shoulder is promptly referred to a rontgenologist. It is to the rontgenologist even more than to the surgeon that this chapter is addressed. The present-day rontgenologist is the diagnostician of the community, not only in bone tumors, but in almost every department of medicine and surgery. He must know all the specialties so far as diagnosis is concerned, and some of them so far as treatment is concerned. His danger at present is in accepting cases referred for treatment by practitioners not qualified to decide for the patient as to whether or not X-ray therapy should take the place of surgery.
Relation of Pathologic Conditions to X-ray Appearances.
As a first step in this study of the Registry cases all the X-rays of the 144 cases were taken out of the envelopes and arranged on tables, classifying them according to this chart from X-ray diagnosis alone. In very few cases was there any difficulty in putting them in their proper places. I also had the same experience with an independent examination of the slides. Then the clinical histories and the written opinions of the pathologists who had examined the slides and the Registry classification of each case were compared. In the main, from whatever angle I approached, I found I could make the diagnosis and prognosis. Either from an excellent X-ray or an excellent slide, and in most cases from an excellent clinical history alone, the diagnosis could be made. Most of the difficulties came from incomplete or poor technique. Very few cases were registered with excellent data in all three respects.
A few cases were doubtful even with excellent technique. Another fact was obvious. If a good X-ray was puzzling, the slide of that case and the clinical history were, too. Such cases have been classed as "Atypical Sarcoma," if I felt tolerably sure that they were cases of primary malignant disease of the bone, although not confident of the variety. Some of the atypical sarcomas are unique and waiting for other similar ones to form a new group. Let us follow the table and first consider the Rontgenological appearances of tumors of the upper end of the humerus.
.jpg)
FIGURE 68. INTERPRETATION OF X-RAY OF OSTEOGENIC SARCOMA
Osteogenic Sarcoma. X-ray and schematic drawing of osteogenic sarcoma. The outline of the shaft still shows within the tumor, which ceases at the epiphyseal line and does not invade the head of the bone. The triangle at the lower margin of the tumor is, in reality, a cuff like a candlestick, made of defensive new bone, which will be destroyed as the tumor progresses downward. The radiating spicules shown in the X-ray are probably formed by the action of tumor cells which are essentially osteoblasts, although they have received the malignant impulse which makes them cease to respect the normal laws of growth. In the dissected specimen of such tumors the outer surface is much more smooth than is suggested by the X-ray, and does not have the prickly roughness which seems to be indicated in this diagram. The reader must not expect to find radiating spicules in all cases of osteogenic sarcoma. Sometimes there is no bone production and very often, as in the next figure, one cannot recognize any radiating structure.
Osteogenic Sarcoma. There were twenty-four which showed fairly typical X-ray appearances of osteogenic sarcoma; i.e., the old shafts were visible in the tumors, which were evidently both intra-cortical and extracortical; there were "reactive triangles" and "sun-ray spicules." These tumors all occupied the metaphysis up to the articular head, the contour of which was not destroyed. These tumors as a rule are enlarged outward beneath the deltoid, but some are almost globular in shape. In two cases in which photographs of the patient were given, the external swelling presented a fusiform appearance, with the greatest diameter distinctly below the region of the tuberosities. In all cases in which we had slides, the histologic type was very clearly osteogenic sarcoma. The diagnosis was further confirmed by the report of death in all the cases but No. 49, traced three years only, and No. 812, traced five years. All but five showed pathologic fractures, and of these five, four were of the "sclerosing" type. Dr. Bradley F. Coley was, I believe, the first surgeon to call attention to the interesting fact that pathologic fracture is more common in the humerus than in the femur, which is so distinctly a weight-bearing bone. (Bradley F. Coley and George S. Sharp. Amer. Jour. Surg., Vol. ix, August, 1930, pp. 251-263.)
.jpg)
FIGURE 69. SCLEROSING OSTEOGEXIC SARCOMA
This case illustrates the fact that osteogenic sarcoma in this region tends to grow outward under the contour of the deltoid, and does not tend to invade the articular head of the bone and the joint
Five cases presented so much new tumor bone that one might be justified in calling them instances of the "sclerosing" type. Only one of these had shown definite evidence of fracture, and even in this case, the fracture was of slight extent. Most of the new bone deposited was to the outer side, so that the contour corresponded with that of a large deltoid. Histologically, the soft parts of these tumors were characteristic of osteogenic sarcoma. The evidence of their belonging to the "sclerosing" variety was chiefly from the X-ray. Death had been reported in all of these cases.
Five cases might be classed as belonging to the osteolytic type of osteogenic sarcoma, with much disintegration of the bone and no bone formation. All of these tumors were very large and very far advanced. In only one was a section obtained, so the diagnosis was not certain in the other four. In their earlier stages they may have shown typical X-ray appearances with radiating spicules, etc., which later were again dissolved by the tumor. In X-ray interpretation, rontgenologists must bear in mind that many tumors cause bone proliferation and then devour the new bone. The reactive triangles at the bases of osteogenic sarcomas are normal new bone with which nature endeavors to check the progress of the disease. In the macerated specimen, it is seen that this triangle, since it is present at the periphery from all angles, really forms a trumpet-shaped affair which holds the old shaft as a candlestick holds a candle. This collar of bone is constantly being absorbed and renewed at a lower level.
So far as this collection is concerned, I do not place much significance on the five cases of osteolytic type, especially since four of the five were not confirmed by slides or autopsy, and all were in advanced stages. Two, at least (Nos. 484 and 643), were in cases of Paget's disease, and such cases are always atypical, and very apt to be of the osteolytic type, both from the X-ray and microscopic point of view. Microscopically, osteolytic tumors are usually very cellular and very actively growing, but occasionally a purely cartilaginous tumor is very osteolytic and advances through the bone as if melting it away. The non-radiable lime salts are completely absorbed and replaced by radiable cartilage, and yet the line between is sharp under the microscope. No. 1,000 is such a case.
Dr. Phemister (Surg., Gynec. & Obstet., January, 1930, p. 234) recently brought up the question of whether chondro-sarcoma should not be separated from the other forms of osteogenic sarcoma as a clinical entity. He feels that if an osteogenic sarcoma is largely composed of cartilage, the natural history of the case is longer and the prognosis of operation better. I do not agree with his point at present, but other members of the Registry Committee do. If we go back to the old nomenclature of chondro-sarcoma, we shall also have to go back to osteo- and fibro- and then to their mixtures. We should wait for a demonstration of some distinct difference in the clinical course of the chondromatous type in its way of responding to treatment before we accept Phemister's suggestion. We have only a handful of cures of all forms of osteogenic sarcoma in all parts of the body, and the chondro-type forms no large proportion of these. It may be that any fully differentiated form, whether osteo- or chondro- or fibro- has a better prognosis than the usual case, which generally contains a mixture of all three intercellular substances. However, this theory is not borne out by the tumors of the shoulder bones, for only one is still living as a five-year cure and this is Phemister's Case No. 812. His other case, No. 1,031, I do not consider a sarcoma, but as a giant cell tumor, and will discuss it later in this chapter. Other than this frail evidence, there is none to encourage his suggestion, so far as the shoulder bones are concerned, unless the group of epiphyseal giant cell tumors is included as showing instances of chondro-sarcoma. In Geschickter's opinion this should be done.
Ewing's Sarcoma. Osteogenic sarcomas of the upper end of the humerus are pretty uniformly confined to the metaphysis as opposed to Ewing's sarcoma, which involves the shaft (diaphysis) from epiphysis to epiphysis. Two cases of osteogenic sarcoma, No. 852 and No. 1,002, extend well down the shaft, but the radiating spicules are much longer than in any cases of Ewing's sarcoma, in which the spicules, if present at all, are only about one-fourth inch in length. One may pretty safely say that most sarcomas involving the shaft of the bone will be Ewing's, and that Ewing's sarcomas do not occur in the upper end of the bone without showing involvement of the major portion of the shaft.
The usual X-ray criteria for Ewing's tumor, broadening of the shaft by separation of the lamellae and the formation of onion-like layers of periosteal new bone as the tumor advances beyond the cortex, are beautifully shown in the cases in the humerus. I am inclined to think that Ewing's sarcoma in the shaft of the humerus very frequently shows fine, short radiating spicules outside the onion-like layers. But the new bone is merely reactive bone.
Ewing's sarcoma outnumbers all the other tumors of the shaft of the humerus. The only other condition with which one familiar with its typical appearance could confuse it, would be osteomyelitis, especially because both of these lesions cause febrile symptoms. The diagnosis is confusing on clinical grounds because in Ewing's sarcoma pain is usually intermittent at first. It usually appears in healthy, rapidly growing children, while osteomyelitis as a rule has a definite history of infection in some other part of the body. Nevertheless, any one who operates for osteomyelitis in any bone should exclude Ewing's sarcoma or be prepared to recognize it. The X-ray appearances of the two are similar, but not alike. When the pain in cases of Ewing's sarcoma is severe enough to make the patient consult a doctor, the X-ray will show well-advanced changes, but in acute osteomyelitis the pain precedes the changes visihle in the X-ray by some weeks.
.jpg)
FIGURE 70. INTERPRETATION OF X-RAY OF EWING'S SARCOMA
Film and schematic drawing of method of invasion of Ewing's sarcoma. The tumor involves the shaft of the bone, invades between the lamellae and destroys the trabeculae even in the cortex. It stimulates defensive periosteal new bone, which it may in part destroy, although new layers form again in defense; hence the "onionlike layers." A cross section of such a bone would show that this process is centrifugal, so that the whole shaft appears somewhat widened
Multiple Myeloma. We may readily dispose of this lesion in a differential diagnosis of pain in the shoulder. The X-ray appearance is characteristic and it does not involve the head alone, but extends down the medulla or forms lacunae in the cortex. It is among the few really endosteal tumors. It is truly inter- and intra-cortical, and advances in the spongiosa and medulla more definitely than is characteristic of any other tumor, even of a cancerous metastasis, the bone tumor which most resembles it in the X-ray. Yet one case of early myeloma in the femur, I recall diagnosing as a cyst! Once having seen a good X-ray of a myeloma and having realized the essential elements of its pathology, one should readily separate it from other tumors of the bone. It is essentially a hyperplasia of marrow cells, not a tumor with intercellular substance. It is multiple in origin and can only arise where there are marrow cells and then dilate the spaces in which these cells normally lie. We know such cells are normal in the medulla and in the spongiosa chiefly, but they may occur in small spaces in the cortical bone. As the hyperplasia in each space—large or small—increases, the spaces are enlarged and break into one another and the intervening trabecule are absorbed. The result is an appearance as if the bone were blown up from inside, as by a series of bubbles, large and small. The periosteum is somewhat stretched and as the process advances, lays down a film of new bone so that a pencilled outline is given to the whole. The bubbles may be single or multiple. The process is quite different from that which takes place in Ewing's sarcoma, where it is essentially invasive and peculiarly apt to be cortical, since the tumor cells penetrate every part of the bone following the lacunae and Haversian canals and separating the lamellae around the circumference, dissolving the bone as they go.
.jpg)
.jpg)
.jpg)
FIGURE 71. INTERPRETATION OF X-RAY OF MYELOMA
X-ray and diagrammatic drawing of a myeloma of the upper end of the humerus. Even little marrow spaces in the cortex have developed foci; the whole upper end of the hone is blown up as if by a mass of bubbles. The method of invasion of this tumor is essentially one of expansion of each little marrow space. In this specimen there were more foci than usual.
Myeloma of the clavicle, which shows the tendency of the tumor to expand the bone as if blowing it up by small bubbles.
The process of dilatation in giant cell tumors is also different, for instead of blowing the bone up with large and small bubbles, as does myeloma in most cases, there is one large bubble which expands by pulsation, destroying all the spongiosa on its periphery until it reaches the resilient medulla on one end and the resilient cartilage on the other. It does not, like myeloma, extend in the marrow, but stops abruptly. I think the reason is that the medulla also pulsates and stops the advance of the tumor. The apparent trabeculae in giant cell tumors are merely ridges in the cortex, not evidence of loculi in the tumor. It is my favorite theory that the origin of all giant cell tumors is a ruptured branch of a nutrient artery which does not clot. Expansion takes place from this single point. Giant cell tumor always arises in spongy bone, myeloma in the marrow of the shaft and also in the spongiosa or cortex.
Giant Cell Tumors. In the head of the humerus giant cell tumor does not behave in a typical way, and my study in 1930 of this group of registered tumors of the shoulder bones resulted in the following paper, which is here reprinted with the permission of the editor of Surgery, Gynec. & Obst. No other tumors of this type were registered in the last 277 cases up to April 7, 1931. (1,060 to 1,335.)
Reprint from
SURGERY, GYNECOLOGY AND OBSTETRICS
February 15 {No. 2A), 1981, Vol. HI, 548-548
EPIPHYSEAL CHONDROMATOUS GIANT CELL TUMORS OV THE UPPER END OF THE HUMERUS
Giant cell tumors of the upper end of the humerus are either very rare or else they should include the nine tumors in the cases I am about to discuss, which in our series have in some instances been called giant cell tumors and in others chondromata, or chondro-sarcomata. Evidently a giant cell tumor affects the upper end of the humerus in a different way from that in which it affects the other long bones. Case 117 registered by Bloodgood is the only one which seems to resemble a typical giant cell tumor, and even in this case very little expansion of the bone is shown.
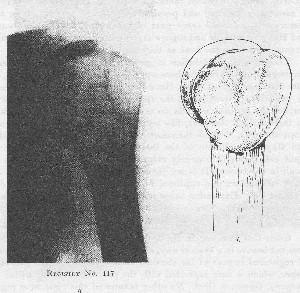
FIGURE 72. INTERPRETATION OF X-RAY OF GIANT CEI.I. TUMOR ARISING IN AN ADULT
Interpretation of Giant Cell Tumor arising in an adult. Diagrammatic drawing representing the probable condition which would be shown by the dissected bone in such a case. Note the biceps groove in both drawing and X-ray. The apparent trabeculations in these tumors are usually only local ridges or thickenings in the outer walls; few, if any, interior compartments exist in them.
There are two other cases, 4 and 556, which are perhaps pure giant cell tumors, but owing to the poor data we have received concerning them, they cannot be seriously considered. I do not know of a single case of typical giant cell tumor in which the growth has expanded the whole upper end of the humerus to the very cartilage of the joint, and which shows the typical trabeculae which are observed in such tumors in other bones. Phemister tells me there is such a specimen at the Presbyterian Hospital in Chicago. It is my belief that the peculiar structure of the head of the humerus makes the picture of giant cell tumor so modified that typical cases do not often occur.
.jpg)
FIGURE 73. INTERPRETATION OF X-RAY OF GIANT CELL TUMOR ARISING IN A YOUTH
These tumors are modified in their structure because the epiphyseal lines are involved in them, and therefore contain irregular proliferating cartilaginous areas, and in these some bone production.
The type of case I allude to in the title is illustrated in the Registry Series by nine tumors of the upper end of the humerus, involving only the portion of the bone in the region of the tuberosities. I wish to call attention to the fact that all the cases in this class are very atypical for either giant cell tumor or osteogenic sarcoma, and that they have a characteristic appearance both by X-ray and in the microscopic slide. It is of interest that the first case (Croxton, Registry 5) has recently been reported by Geschickter and Copeland as a sarcoma.1 On the other hand, Kolodny has reported the same case as a giant cell tumor and illustrates his book (Figs. 88, 89, and 98) with photomicrographs and X-rays from it. The last case in the group, 1,031, has been recently reported by Phemister2 as one of chondro-sarcoma. Three of the other cases were registered by Coley. Since these men have given serious study to the subject, I cannot lightly take the position that their conclusions have been erroneous, and that in reality, their cases were not malignant but were benign giant cell tumors of this chondromatous type. However, the intermediate seven similar cases in the Registry present such uniformity in the long history prior to operation, the ages of the patients, the good results following conservative treatment, and the unanimity of X-ray and microscopic appearance, that I am personally convinced that all the cases, theirs included, had essentially benign tumors. I believe that this group of tumors is a clinical entity which the surgeon should bear in mind when confronted with tumors of the upper end of the humerus.
1 Arch. Surg., 1980, May, pp. 731-733.
In regard to one of these cases (391), of which we have no X-ray, registered by Coley, but which had been operated on in January, 1915, at the University of Michigan, Ewing wrote on the Registry Classification sheet as follows:
"Dec. 18, 1923. This appears to be one of the cases of giant cell tumor associated with the absorption of cartilage. Such tumors are generally found at the head of the humerus. The giant cells are rather numerous, typical epulis type, and most numerous about blood spaces. The accompanying cells are peculiar, and are rather large polyhedral granular cells occurring in sheets and clumps. In some areas the giant cells are missing and the polyhedral cells appear exclusively. There are several small foci in which there is dark, staining fibrillar or partly hyaline material, which appears to be degenerating cartilage. There may be some new formation of this imperfect cartilage. There is no sign of bone formation. It does not resemble any of the well-known forms of osteogenic sarcoma. Tumor is relatively benign, but probably more active than most giant cell tumors."
2 Surg., Gynec. & Obst., 1930, 1. 216.
.jpg)
FIGURE 74a
Registry 391. Registered by Coley, but had been operated on at the University of Michigan, in January, 1915. The patient, a boy of 15 years, had a tumor of the right shoulder. He was unable to raise his arm. Pain had been present for eight months. He gave no history of injury. He was treated afterward with toxins. The slides show the characteristic appearance of these tumors. No X-ray. This is the case on which we quoted Ewing"s pathological report. Well in October, 1923.
The line in italics in which Ewing says, "Such tumors are generally found at the head of the humerus," shows his recognition of this type of tumor. He has also alluded to them in his paper at the 1929 London Congress under the caption of "Calcifying Giant Cell Tumors," as follows: "I also feel that these tumors are essentially giant cell tumors, and that one must not be deceived by the appearance of chondro-sarcoma which they give."
The much-discussed Croxton case, Registry 5, was that of a boy of 16, registered by F. G. Bunts, Cleveland, one of the first cases in the Registry Series. There has been much argument about this case among those interested in the Registry. Bunts consulted Bloodgood and the case appears in Bloodgood's writings as P. N. 26792. Bloodgood favored a pre-operative diagnosis of benign tumor, but changed this diagnosis to central sarcoma after seeing the specimen. Bunts, however, using his clinical judgment at the operation, decided to treat the case conservatively.
.jpg)
FIGURE 74b SHOWING TYPICAL APPEARANCE OF ONE OF THESE TUMORS AFTER CURETTING
Registry 5. Bunts first saw the case May, 1919, five months after the boy had hurt his shoulder while wrestling. During these months, there was a history of the shoulder having slipped out of place and readily slipping back again into the socket. In the last two months there had been much pain, especially at night. There was also scapulo-humeral spasm. Bunts first treated the shoulder conservatively with a rubber bandage, but in October, 1920, he had X-ray pictures taken which showed the tumor. He then consulted Bloodgood, and operated on October 11, 1920. The patient was reported to be well ten years later.
He did a very thorough curetting of the tumor and packed with gauze; eight days later he cauterized with zinc chloride, implanted radium, used postoperative X-ray and Coley's toxins. The patient has remained well. Geschickter and Copeland, in their recent article of 1930, still consider the case a sarcoma.
.jpg)
FIGURE 75a
Registry 86. Registered by C. C. Simmons, of Boston. A boy of 13 years had had for one year, a hard, smooth tumor, the size of an egg. Curettage was done August 6, 1918. The X-ray picture which was typical of this kind of tumor was poor and was probably taken after curetting. The slide is a good example of this kind of tumor. It presents more giant cell tissue than some of the others. The giant cell tissue verges on the true giant cell tumor type. Patient was well in November, 1922. No further note.
In the early days of the Registry, it was considered sarcoma by Ewing, Mallory, Wolbach, Wright, White, Fox, Taylor, and Phemister. Later, Ewing and Bloodgood changed their opinions and agreed with Graham, Stout, Connor, Morton, and the writer, who had considered it a giant cell tumor. It seems to me that in consideration of the other eight cases here presented and the outcome of this case that the diagnosis of giant cell tumor is the correct one. The nine cases may be summarized as follows:
SUMMARY OF NINE CASES
X-ray characteristics. These giant cell tumors or chondro-mata( ?) of the upper end of the humerus lie in the angle between the upper and lower epiphyseal lines, i.e., in the greater tuberosity, and are checked at the epiphyseal line of the articular head. Fractures of normal bones in this region are very apt to separate the portions of the bone at the lines of cleavage of the old epiphyses. It appears that in normal bone there is a line of cleavage separating the portion of the bone which is covered with cartilage from the rest of the head, and that this line of cleavage persists long after the epiphyses have united. It may be this line of resistant bone which keeps these tumors from reaching the articular head. At any rate, these tumors do not, as do giant cell tumors in the neighborhood of other joints, actually destroy the bone to the very cartilage. Thus these tumors affect the bone after the manner of osteogenic sarcoma and one always sees in the X-ray picture a small portion of normal bone near the articular surface. This appearance in the lower end of the femur is very characteristic of an osteogenic sarcoma, but it should be discounted when it is found near the head of the humerus. In other words, these peculiar tumors break the rule of giant cell tumors in other bones of progressing through to the very cartilage of the joint, and in the head of the humerus do not extend much beyond the epiphyseal line.
They do not present the characteristic trabeculations which are seen in the X-ray picture of giant cell tumors in other bones. Instead they have a fluffy, "cotton-wool" look. After curettement, they present a fairly characteristic appearance, as if the tuberosities had been gnawed away, thus leaving the articular head and a very definite neck of bone on the inner side. Before curettement, the X-ray examination shows that there is a rather sharp line of demarcation separating the irregular, flocculent mass occupying the region of the greater and lesser tuberosities from the articular head, the inner portion of the neck of the humerus, and the rest of the shaft. A very characteristic feature in all the X-ray films is a buttress of apparently thick, normal, cortical bone on the outer portion of the shaft just below the tumor.
.jpg)
FIGURE 75b
Registry 603. Registered by Coley. Male, aged 15 years, was admitted to hospital February 18, 1924. Six months ago he had pain in the right shoulder, followed by stiffness three months later, with some swelling. He had had electrical treatments with no relief. He was treated with X-ray by Herendeen, and was reported well in July, 1931. No slides were made. X-ray films in this case indicate a certain amount of separation of the greater tuberosity, but are fairly characteristic of the group. No history of injury was elicited.
This appearance suggests that the tumor has been of quite long duration and nature has supplied reactive bone to strengthen the cortex below it. There is also a thick endosteal layer of bone especially evident in Phemister's case 1031, which had been curetted twice before the resection. The outer buttress is not in appearance like the so-called "reactive triangle,"'in which there is a triangle between the raised periosteum and the old cortex. It is much more dense and extends much farther down the bone. The buttress is solid and is merely an increase of normal cortical bone, with no invasion of tumor tissue between the old cortex and the periosteum as we see in osteogenic sarcoma. All nine of these tumors are comparatively small, none being twice as large as the normal head of the humerus.
.jpg)
.jpg)
FIGURE 76
Registry 1031. Registered by D. B. Phemister, in August, 1919. Male, aged 22 years. Three and a half years ago he had slight pain, followed by slight limitation. Operation was done two years ago, by another surgeon; the area of reduced density in the tuberosity being curetted. Symptoms soon recurred, a second curetting was done but no sections were made. Limitation of movement and pain became worse. Phemister resected the upper six inches of the humerus, and applied a bone graft in August, 1919. The outcome was successful, and the patient was well eleven years later. The X-ray is fairly typical of this condition and the slide is very typical. The relative proportion of chondromatous material to giant cells is greater than in the other cases, but this case was operated upon twice before, and had in the meantime passed the age of epiphyseal union. The X-ray was made from the specimen after removal.
The microscopical appearances are chiefly distinguished by the presence of peculiar epithelioid cells which merge into a low-grade type of cartilage cell on the one hand, and into the cells of the tumor on the other. Sometimes the newly formed cartilage forms the bulk of the tumor, and sometimes a tissue indistinguishable from giant cell tumor occupies most of the space. The gross curettings are composed partly of red, friable tissue and partly of whitish, sago-like bits of material or frank cartilage. Sometimes the bulk of one of these tumors is almost wholly cartilage. Perhaps these instances are in slightly older patients, near or just beyond the age of epiphyseal union, e.g., Phemister's case 1031. Sometimes there is a deposit of calcium in the cartilage, and new bone formation. It is very likely that some cases may be complicated by infraction and callus.
We frequently find newly formed cartilage and bone toward the periphery of a giant cell tumor, and we sometimes see in giant cell tumors in other parts of the body small areas which correspond to the peculiar tissue seen in these tumors of the humerus. However, we seldom see, in tumors of the other parts, the bulk of the tumor made up by this low-grade cartilage and epithelioid cells.
.jpg)
FIGURE 77
Registry 174. Registered by Coley. No operation was done and hence no slides were made. Patient was a pregnant female, colored, aged 24. She was admitted to Memorial Hospital, February 1, 1922. She had had pain, with increasing severity, for six months, and a tumor soon followed, July, 1921. The method of treatment was not stated. In August, 1930, Ewing reported that she was well. The notes were very brief. The X-ray is fairly characteristic of this type of tumor.
Since we may find similar tissue in true osteogenic sarcomata which involve the epiphyseal lines in this region, it cannot be too strongly stated that the presence of this tissue does not prove that the tumor is benign. I merely wish to make the point that this peculiar tissue probably indicates a benign process and together with the characeristic X-rays and clinical history would justify conservative treatment. In fact, I believe that characteristic X-rays alone are sufficient evidence to justify the institution of radiotherapy without incision. It seems to me that tliere is reason to believe that if one of these patients were treated with the X-rays alone, the ultimate result would be better. Unfortunately, there are no detailed notes on the end-result of Case 174, which is the only one in which no incision was made.
.jpg)
Registry 816. Registered by E. T. Dickinson, Greenville, North Carolina. A girl of 17 years, about a year before entering the hospital, noticed a dull pain in the right shoulder. The pain had increased until she could barely use the arm at all. Abduction to more than twenty degrees was impossible. Operation was done October 5, 1926. The tumor was curetted and swabbed witli zinc chloride. The supraspinatus and subscapularis were removed and sutured back to the rims of the head. After operation Coley toxins and X-ray treatment were given. She was well, with some limitation of arm movement, in August, 1930. X-ray pictures before and after operation were typical of this kind of tumor. The slides were very typical. There was more bone formation than usual. There were areas of giant cells mixed with cartilage and bone.
Clinical points. The age may prove of importance in diagnosis, when we get a larger series. It is highly probable, as suggested by J. H. Wright, that this cartilage-like tissue is derived from the epiphyseal line. It will be observed that the ages in the cases here presented were in the neighborhood of the time when the epiphyseal lines were still present (given as twelve to twenty-four, but the tumor must have begun earlier in each case). One must bear in mind, too, that the epiphyseal lines in the region of the head of the humerus occupy a relatively larger part of the bone than do such lines in other situations, because there are three separate centers of ossifications: one for each tuberosity, and one for the head. The upper surface of the diaphysis, adjacent to the epiphyseal line, is cone-shaped.
.jpg)
FIGURE 79
Registry 815. Registered by W. A. Clark of Pasadena, California. A boy aged 20 years, colored, had pain in his arm which began in November, 1926. The arm was stiff. He was operated on March 10, 1927, at which time the entire upper end of the humerus was resected. He was working October 13, 1931. The X-ray was very typical, as was the microscopic slide
Another clinical point is the relatively long histor}' of symptoms prior to any operation, or the formation of a large tumor, i.e., at the least, six months and an average of over a year. It is of interest to us also that the early symptoms are very similar to those of subacromial bursitis, i.e., pain and restriction of motion. As I have never taken care of one of these patients myself, I cannot speak positively of the early symptoms, and the notes in our cases are very meager, but all mention pain and restriction. However, since these tumors lie just beneath the bursa, it is highly probable that they do produce a bursitis by crowding the enlarged tuberosities under the acromion. There should be a question of this diagnosis in cases with symptoms of subacromial bursitis in persons under twenty, for subacromial bursitis is rare at this time of life, and these peculiar tumors occur only at this time of life.
Since all twenty-four patients with true osteogenic sarcoma of the head of the humerus are dead or very recently registered, a most important clinical point in the nine cases reported here is the history of recovery without amputation of the arm. In three of our cases curettements were done, excision was done in one case, resection including the head of the bone was done in three cases. The two others had no operations. Coley's toxins were also used in Registry cases 5, 174, 391, and 816.
I have described these cases in some detail for two reasons. First, because I believe they represent a subordinate clinical entity which should be recognized in the literature; and second, because they are among the few bone tumors which lie in direct contact with a part of the subacromial bursa and give bursal symptoms. In fact, an operator could not thoroughly curette or excise one of them without opening the bursa. If the growth were malignant, one could hardly fail to leave some cells in the bursa. That seven were thus curetted or excised with the bursffi opened (and probably also the joint), and extension of the disease did not result, seems strong evidence that the tumors were essentially benign.
Another point is that in our nine cases the clinical judgment of the surgeons in charge was evidently in favor of conservative treatment, for no amputations were done in spite of the pathology.
.jpg)
Registry 902. Registered by H. B. Thomas, Chicago Research Hospital. A girl of 14 years had had pain and difficulty in putting on her coat for a year. She gave no history of trauma. Some swelling was present. She had had some chiropractic treatments. She was operated upon by Hedblom, March 10, 1927, at which time the upper end of the humerus was excised. June 27, 1927, the upper end of the Iefl fibula was transplanted. The wound healed with primary intention. She was well, July 27, 1931, with no sign of recurrence. The slide and the X-ray picture were very typical.
Treatment. Since the cases are few in number and the treatment has been outlined in each case, the reader may take his choice of methods. I think I should incline toward mild X-ray therapy, but if I decided to operate, the procedure followed by Dickinson (Registry 816) appeals to me as the best, namely, to excise the tumor and to suture the short rotators to the defect in the head of the humerus. Unfortunately, we have no details about the function of the arm in these nine cases. All are said to have useful limbs, but the degree of usefulness with and without bone grafts cannot be compared without examination of the individual cases.
It is highly probable that similar giant cell tumors may arise in patients between ten and twenty years, in the region of the other skeletal epiphyses, especially in the homologous region of the great trochanter of the femur. I believe that Case 277 is such an instance, although in the Registry it is carried as a case of osteogenic sarcoma.
With regard to the name by which to designate this type of tumor. I have used the adjective epiphyseal because I believe that these tumors are characteristic of the period of life when the epiphyses are uniting and that their peculiar cells arise from the epiphyseal cartilage. I have used the adjective chondromatous as descriptive of their histology. I believe that they are essentially benign giant cell tumors, and thus that part of their name is justified. Yet I am not satisfied with such a long, cumbersome name. Ewing speaks of them as calcifying giant cell tumors, but that does not seem to me descriptive enough. We must find a name which will not tie the tongue, but it should associate adolescence with this puzzling type of lesion.
(End of reprint.)
Metastatic Cancer. The advance of a malignant metastasis may mimic the methods of invasion of any of the primary bone tumors. It usually begins in the neighborhood of the nutrient artery or in one of its branches as an embolus. The cells multiply and have an osteolytic and invasive power. The bone melts before them or, if they are slow growing, piles up new bone to check their advance. Rapid vascular metastases may dilate the bone by pulsation as do giant cell tumors. If the osteolytic quality of the cells is predominant, a local defect is produced in the bone and transverse fracture occurs. If there are multiple emboli, the bone may be riddled by many foci which all advance together and melt into one another as do the lesions of myeloma, but the X-ray appearance is not quite like the latter.
The very diffuse form of cancer involving the whole bone without changing its shape, is probably due to lymphatic extension. Although many writers have denied the existence of intraosseous lymphatics, Kolodny believes he has proved their presence in bone. (Kolodny, Anatole. The Relation of the Bone Marrow to the Lymphatic System. Arch, of Surg., 1925, Vol. II, pp. 690-707.)
On the whole we may say that cancer is so variable in the way it attacks the bone, that any unusual X-ray of a bone tumor should arouse the suspicion of metastasis. In an adult, a localized osteolytic tumor in the shaft of the humerus or involving the upper end of the bone from the mid-shaft upward, will usually prove to be cancer. In our table, it will be seen that all six cases of metastatic cancer occurred in the shaft of the humerus, and none in the ends. One case probably started in the shaft not far above the nutrient foramen and the whole upper third of the bone was destroyed. While this series is very small, it accords with my general experience, which is, that a tumor of the upper end of the humerus, without involvement of the shaft, will rarely prove to be a metastasis. There are exceptions, however. In generalized carcinomatosis of the skeleton the humerus is, of course, involved. Myeloma may involve the shaft. Metastatic cancer seems to be the only lesion which invades the head of the bone to the very cartilage.
Of the five cases confined to the shaft, two present dilatation of the cortex, while the other three show only localized bone destruction, without dilatation. The dilatation probably depends upon the vascularity of the tumor, for the blood pressure working from within the bone destroys the firm cortex after the manner of an aneurysm,or of a giant cell tumor. Hypernephroma metastases frequently have this expansile quality. As in giant cell tumors, the periosteum may keep endeavoring to surround the growth with new bone, and unless the advance of the tumor is rapid, maintain a thin bone shell about it.
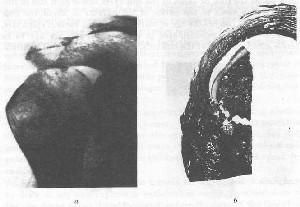
FIGURE 81. METASTATIC AIKTASTATIC CANCER INVADES THE MARROW SPACES OF THE ARTICULAR HEAD WITHOUT CHANGING THE CONTOUR
a. Metastases of cancer of the breast. Reduced one-half. Both the head of the humerus and the acromion are involved. The opposite shoulder was also similarly affected, as were many of the other bones, but the outlines as shown by X-ray were not dilated or otherwise changed. Notice that the involvement, as shown in radiability, extends into the articular head of the humerus.
B. Photomicrograph of section through the attachment of the supraspinatus tendon in a case of cancer of the prostate with diffuse skeletal metastases. Enlarged two diameters. The section was broken when being cut. The marrow spaces are filled with cancer cells.
In films which show disorganization of the interior of the articular head but without change of outline, the presumption should be that the disease is cancer, for not only does cancer generally involve this region, but snrroma very rarely passes the old epiphyseal line.
It is a fair working rule that a localized tumor of the mid-shaft will prove to be a metastasis, although occasionally a myeloma (No. 676) or an osteogenic sarcoma (No. 156) occupy this position.
Benign Osteogenic Tumors. This heading includes tumors which formerly appeared in the literature as osteomas, chondromas, exostoses, ecchondroses, enchondromas, and the combinations of these tumors with fibromas and myxomas, e.g., fibro-myxo-chondro-osteoma, etc. These tumors are as a rule congenital, but may not be noticed until about the time of union of the epiphyses and seldom late in life. Usually they come to the notice of the parents at about the time when the child reaches the age of ossification of the various epiphyses. They are usually pedunculated in other bones, but are apt to be sessile about the head of the humerus. They may be single or multiple.
.jpg)
FIGURE 82. BENIGN OSTEOGENIC TUMOR
Registry No. 31
Benign osteogenic tumor of the upper end of the humerus with the X-ray projection. Although poor, the X-ray is presented because it is taken from the bone shown in the photograph. This form of tumor is not uncommon in this situation. In the writer's opinion radical excision of the tumor, leaving only enough shaft to form a reasonably strong bone, is indicated, rather than total excision.
The tumors are not invasive, and while they push aside other tissues, they do not either destroy or penetrate them. The proportions of combinations of osteo-, fibro- and chondro- elements appear to have little significance, except that the softer the cartilage becomes, tending to be myxomatous in character, the more rapid the rate of growth is likely to be. These tumors are not uncommon near the head of the humerus, and it is rather remarkable that only one instance of a benign osteogenic tumor of the humerus has been registered. We do not ask for registration of these cases, but one would think that a considerable number would have been sent us, because they had been mistaken for malignant tumors.
The one instance which was registered, No. 31, although quite a small tumor, was excised by a surgeon under the impression that it was a sarcoma, and his diagnosis was confirmed by the hospital pathologist. In this particular case, the members of the committee have never seen the slides on which the diagnosis of sarcoma was made, for although the surgeon was quite willing, the hospital authorities did not wish the slide taken from the laboratory to be recorded with the case. We therefore cannot say positively that the tumor was benign. We can only judge from the X-ray which is here reproduced, and from the clinical fact that there was complete recovery after excision—the patient being reported well nine years later. The X-ray is very typical of the sessile tumors which occur in this region. Complete removal was perhaps wise, although the tumor might never have caused metastasis. Thorough excision of the base should be as effective.
The age of the patient is an important factor in deciding whether to operate in the case of such a tumor. My opinion is that operation should be postponed until after the epiphyses are united, for it is quite likely that the tumor will cease to grow at that time. Rapid rate of growth, or growth after the twentieth year, would speak for excision.
So far as benign osteogenic tumors are concerned, I shall have to draw on my own experience rather than on the recorded data of the registered cases. I vividly recall, before the days of the Registry, two exaggerated cases of such tumors of the upper end of the humerus which I had great difficulty in removing. It is one of the characteristics of this type of growth that it tends to extend along the fascial planes without invading the tissue, and if the tumors are large, one finds the muscles, nerves, and vessels buried in channels in the growths. I also have had experience with similar tumors of great size in other bones and I believe that it is of importance, if one operates on these tumors at all, to be very thorough in removing the base of the pedicle through the whole cortex. One should be very careful to remove from the tissues every particle of chipped material in case one has to take the tumor out in pieces. When these tumors are pedunculated, their removal is not difficult, as they are not adherent to any tissue, and usually shell out easily, after the pedicle is divided. Often their surface is covered with cartilage and over this is an adventitious bursa on which the soft tissues and muscles slide.
The operative difficulties will come in those tumors which are sessile and are so large that they have branched between the normal fascial layers and surround the anatomic structures. In the two cases above alluded to, the deltoid was detached from its tubercle and turned upward over the shoulder. The humerus was then sawed directly across, and holding the lower end of the upper fragment, the nerves and vessels were dissected from their canals in the tumor, which was removed piecemeal with the whole upper end' of the humerus. This very extensive excision was accomplished in both cases without dividing any of the important structures, but it necessitated removing portions of the tumor with a hammer and chisel, and much chipping of the tumor into small bits which were as far as possible removed. At the end of the operation, the deltoid was resutured to the upper end of the distal fragment of the humerus. Both patients obtained remarkably useful arms, having very nearly as much function as the classical cases of excision, where only the articular head of the humerus is removed.
One of these cases was that of an extremely stout woman with a very large tumor. In spite of my greatest care to remove chips of the tumor, bits of cartilaginous material remained entangled in the tissues, between the joint and the distal fragment. Many oi these bits of tumor tissue afterward grew independently, and for some years I occasionally had to remove some of the bits which had grown to be the size of robins' eggs. They were always definitely encapsulated. These secondary tumors, on section, were almost pure hyaline cartilage. Eventually, so many of these bits recurred, and their consistency became so myxomatous, that I did a shoulder-girdle amputation. It happened that Dr. Bloodgood came to Boston within a few days after this, and I showed him the specimen before he left. Responding to his exemplary enthusiasm, I presented the limb to him. The picture remains with me of enthusiastic Joe Bloodgood with this stout shoulder and arm wrapped in brown paper, stepping aboard the night train for Baltimore.
Although an exaggerated case of its kind in regard to the size of the tumor, and the clear character of the cartilage in the implantations, it is only an example of a fairly common type of tumor which is benign, for this patient is still living nine years since the last operation. I have seen other cases in which, owing to the fact that the operator had not thoroughly removed the pedicle of the tumor, recurrence at once took place. Cases are on record where these tumors at first are histologically of a distinctly benign character, and have become true osteogenic sarcomas after repeated ineffective surgical measures, or even where no surgery has been done.
Many of these pedunculated, osteo-cartilaginous, benign tumors are multiple. I have been able to follow one of these multiple cases over many years (Registry No. 343), and have seen the individual tumors take on rapid growth and become histologically malignant tumors. The poor fellow had, in all, three limbs amputated, but ultimately died of acute appendicitis with peritonitis. This case does not appear in the table because it is tabulated with the lower extremity. In one case (Registry No. 1016) one of the tumors appeared in the unusual position of the center of the shaft of the humerus. As a rule, operation should not be done in these multiple cases, until the tumor renders the limb inferior to an artificial one. Even when rapidly growing they are not very malignant so far as metastasis is concerned.
Personally, I am inclined to think that the Registry should recognize less sharp divisions between osteogenic sarcomas and benign osteogenic tumors. We should have a Borderline Class, which should include such cases as the two mentioned above. Some of these cases are certainly borderline, and I think it is the failure to recognize this borderline class that gives some surgeons and pathologists the excuse for using the word "chondro-sarcoma." The prognosis will depend on the surgical circumstances which attend the operation, as to whether the tumor can be excised entirely with the cortical bone from which it springs. The histologic criteria which help to form a prognosis in these borderline osteo-chondromatous tumors are not distinct, and depend on one's estimate of what degree of distortion normal cartilage cells may assume without becoming malignant. Mitotic figures will not help us, for we do not find them in cartilage cells. The clinical history, X-ray and gross pathology are of more importance than the histology. The pathologist should be able to see the extent of involvement shown in the X-ray before being asked to make a prognosis. If the X-ray shows intra- as well as extra-cortical involvement, malignancy is more likely. The size of the pedicle is important.
In the multiple cases some of the tumors may be intra- and some extra-cortical. If a tumor is extracortical and also intracortical, suspicion of malignancy is aroused. Flocculent deposits of calcium near the periphery in these borderline tumors give a characteristic appearance in the X-ray.
Sarcomas Occurring in Paget's Disease. Only two cases of the twenty-four osteogenic sarcomas of the upper end of the humerus (No. 484 and No. 643) were over fifty years of age. Both of these patients had Paget's disease. This concurs with the finding which I have mentioned elsewhere, that most cases with osteogenic sarcoma, who are over fifty years of age, have Paget's disease of the skeleton. This conclusion was drawn about five years ago, after a review of the whole Registry series, including all bones. Since then, I have seen a few, but very few, exceptions. Of the seventeen cases of osteogenic sarcoma of the upper end of the humerus registered since 1932, there were three of about fifty. All three had signs of Paget's disease of the bones. Search for signs of Paget's disease in any case of bone tumor in patients about fifty, and search for sarcoma in every case of Paget's disease, for about fourteen per cent of all cases of Paget's disease develop it. (Sarcoma Complicating Paget's Disease of the Bone. Clarence E. Bird. Arch, of Surg., June, 1927, Vol. 14, pp. 1187-1208.)
The histology of the sarcomas that develop in Paget's disease is varied and not typical. In one of our cases (Reg. No. 297), the slide resembles that of a benign giant cell tumor. This case is the only Paget's case in the Registry series in which the slide does resemble a giant cell tumor. Most of the other cases are quite atypical in structure, but their intercellular substance is distinctly osteoid, and by X-ray they are usually of the osteolytic type.
The facts that (1) osteogenic sarcoma is usually found in youth; (2) Paget's disease is seldom found before fifty; (3) less than one in 100,000 normal people have bone sarcoma anyway; (4) fourteen per cent of cases of Paget's may be expected to have it; (5) Paget's disease shows an instability of bone metabolism with enlargement accompanied by loss of lime salts; should give a medical Sherlock Holmes the key to the mystery of sarcoma.
Inflammation.
Under the heading "Inflammation" of the upper end of the humerus, we have six cases. All these six tumors were in our opinion cysts, although they were registered with the idea that they were sarcomas, or giant cell tumors. It may well be disputed whether cysts are to be classed as tumors or inflammation. All these cases, and practically all cysts that I have seen which were not registered, have been in the same situation in the metaphysis and limited by the epiphyseal line, for they nearly always occur in young people, usually under ten years. In all six cases, a pathologic fracture without much displacement had occurred. Pathologic fracture appears to be the rule in these cysts, and repeated fractures may be sustained, but the amount of displacement is very little. A patient may even have a cyst in childhood which later leaves the bone weak, so that pathologic fracture occurs again after the age of epiphyseal union. X-rays in such cases are quite deceptive, for the walls may have become quite thick.
.jpg)
FIGURE 88. CYST OF THE UPPER END OF THE HUMERUS
An old bone cyst in which repeated infractions and healing had occurred.
Very frequently the cyst is not noted until a fracture occurs. The X-ray appearance is so characteristic in these bone cysts, and has now become so well known, that there is little danger of confusing the lesion with any other, except giant cell tumor. The amount of anxiety caused by one of Ihese cases has changed very much in the last decade, for ten years ago it was not at all unusual for bone cysts to be misdiagnosed as sarcomas, and to cause a great deal of discussion and consultation. Dr. Bloodgood should be credited with much of this improvement, for he has for many years reiterated the diagnostic points which distinguish cysts from sarcomas. Even today, it is always with a sense of responsibility that one decides against operation in one of these cases, because the penalty of mistaking an osteogenic sarcoma would be so great. It is a fact, however, that reliance can be placed on the X-ray. In the case of a child, a good, clear-cut picture of a central tumor, extending for several inches below the epiphyseal line, slightly dilating the bone, with an abrupt concavo-convex outline on the lower medullary end, almost certainly indicates a bone cyst. The bone cyst is unlike the epiphyseal, chondromatous giant cell tumors of the humerus in that the latter are between the epiphyseal lines and do not involve the inner contour of the neck, and occur in the teens rather than before ten. I do not know of any case of a giant cell tumor in the upper end of the humerus below the epiphyseal line, but in all the cases of cysts which I have known, that had any operative interference, there was a greater or lesser zone of tissue, resembling giant cell tumor lining the bone, so that many have been classed as giant cell tumors.
Geschickter (Arch, of Surg., August, 1929, Vol. 19, pp. 169-271) has produced a very interesting theory, on a parallel of the normal method of cartilage absorption, for the common origin of cysts and giant cell tumors. I agree in the idea of their merging, but I am more inclined to feel that their origin is generally due to intraosseous hemorrhage from a fissure fracture, dividing a nutrient vessel in the spongiosa. I feel that the difference between cysts and giant cell tumors is probably connected with the age of the patient and the condition of the bone near the epiphyses. Apparently in cysts the artery is soon occluded, and the defect, instead of being filled with proliferative endothelium (which to my mind the cells of giant cell tumor are), through which the blood corpuscles circulate, becomes filled with serum, and has a lining membrane surrounding it, often partly composed of a tissue sjmilar to giant cell tumor.
No tumors of the upper end of the humerus have been sent to the Registry which we thought were of an inflammatory nature, except the cysts. As a matter of fact, in my experience apart from the Registry, I have rarely seen in this region cases of inflammation, even including osteomyelitis and fracture, which simulated real neoplasms in the X-ray. Osteomyelitis in this region in adults must be a very rare condition.
There remain, in the first column of the table, the Atypical Sarcomas and "Cases Discarded" on account of poor data. It would be out of place to attempt to draw conclusions from either of these classes of cases, but we may at least find some encouragement, for a few of the atypical cases of undoubted malignancy are well and will be considered under prognosis.
Shaft of the Humerus. (Second Column in Tables.) Following the policy of relating the contents of this book to lesions in the neighborhood of the subacromial bursa, I shall not discuss tumors of the middle and lower third of the humerus. The reader may readily see the comparative rate of occurrence of these by reference to the chart, and if his curiosity tempts him further, he may send to the Registry for the envelopes of the cases in any particular cross-section of the chart. This gives me an opportunity to say that it is a policy of the Registry to permit any qualified person to study the Registry series and to use the material for his surgical papers as I am using the present study for this book.
The chart confirms the current belief that tumors in the long bones are more common in the ends of the bones toward which the main nutrient arteries point. The tumors of the upper end of the humerus stand in relation to those of the lower end as fifty-five to eleven.
Tumors of the Clavicle.
Only tumors of the outer end of the clavicle concern us, and it appears that following the nutrient foramen rule, more than half of the tumors of the clavicle occur in the outer end. We have in the Registry only a small series—eleven in number. The tumors of the clavicle, as a whole, follow the general rules as laid down for similar tumors in the other bones. It is not difficult to diagnose from the X-ray the osteogenic sarcomas on the principle of the presence of the old shaft in the tumor and the other criteria spoken of in the humerus. The two Ewing's tumors are nearly exactly alike, and have the same characteristic form of invasion of the bone as do these tumors in other regions. The myelomas and giant cell tumors are also very typical in the way they affect the bone. In other respects, this small series of tumors of the clavicle yield nothing of importance for record.
Tumors of the Scapula.
Unless they were in the acromion or coracoid, tumors of the scapula would not be in relation with the bursa. We find that the rest of the bone is much more susceptible to tumors than is the acromion process. However, we have a very good example of each of the typical tumors in the acromion, and furthermore, the prognosis appears to be good, for none of the six cases recorded, whatever the variety of the tumor, have yet been reported to have died.
In one of the cases I personally had the clinical responsibility. A young woman (Registry No. 392) with a conspicuous tumor of the acromion was referred to me by the surgeon who had explored the tumor and found it of the giant cell type, although the pathologist considered it malignant. J wrote this surgeon that I thought I should have to do a shoulder-girdle amputation, but that Ewing and Heren-deen had recently been using X-ray treatment with some success in this type of tumor, and I thought it was only fair to try the X-ray before removing the arm. Dr. L. B. Morrison kindly undertook the X-ray technique. For a few months I had much worry. The tumor swelled and softened until it seemed it must break the skin. I barely withheld myself from operating, but felt that it was now too late, and we must trust the X-ray and Ewing's statement that while these tumors appeared to grow worse following the use of the X-ray, they afterward shrank and the bone returned to approximately a normal condition. The result, six years later, is shown in Fig. 85. The patient is well. During this period of time this method of treatment has become accepted, but the course of my first case was followed with anxious attention.
.jpg)
FIGURE 84. ANGIOMA OF THE SCAPULA
The glenoid and coracoid process are involved. The peculiar radiating striation seems to be characteristic of the method in which cavernous angioma destroys bone.
Angioma.
Cavernous angioma of bone is rare, but there is one instance in this series with a very beautiful X-ray which illustrates the manner in which this condition attacks the bone. The tumor has involved the whole glenoid region, invading down the acromion to within an inch of its tip. A very complete account of what is known regarding cavernous angioma of the bone will be found in the Journal of Radiology. (Paul C. Bucy and Charles S. Capp in Amer. Jour, of Rontgenology, January, 1930, Vol. 23, pp. 1-33.)
Prognosis of Bone Tumors About the Shoulders.
The table speaks for itself, for those cases are underlined in which death has been reported. The cases not underlined will be alluded to below. It goes without saying, that cases of cancerous metastasis are always fatal. The prognosis of multiple myeloma is little better, except that it is more favorably influenced by radiation.
From the table we see that prognosis in osteogenic sarcoma of the upper end of the humerus is certainly very bad. Only two cases (No. 49 and No. 812) were living when last heard from. Case No. 49, registered by Dr. Emmet Rixford of San Francisco, had a large osteogenic sarcoma of the upper end of the humerus. A shoulder-girdle amputation was done on June 11, 1901. The patient was well on April 16, 1904, and has not been heard from since. Onset of the disease in this patient was two years prior to the amputation, so that the patient may be considered to have been alive five years from the onset. Five years from the onset and three years from the date of operation are encouraging, because they are longer than the average duration of life for osteogenic sarcomas of the upper end of the humerus, namely, about two years. Even among the five cases each of the sclerosing and osteolytic types, there appears to be no better prognosis than in the average type. The death of every case of these types has been reported.
.jpg)
FIGURE 85. GIANT CELL TUMOR OF THE ACROMION BEFORE AND AFTER X-RAY TREATMENT
Films of case referred to on page 454, taken before and after treatment. Before treatment the acromion process appears to be nearly destroyed and shows only as a faint outline. In the second film the structure of the acromion appears to be nearly normal. In such tumors, although they appear to be quite diaphanous, the periosteum is capable of regenerating new bone just as it is when a piece of bone is excised subperiosteally.
There may be a slightly better prognosis for osteogenic sarcomas of the chondromatous type, as alleged by Phemister in Surg., Gynec. and Obst., January, 1930. One of the cases (No. 812) has been reported in full by Phemister. This was a large tumor of the chondromatous type of osteogenic sarcoma and is alleged to have survived shoulder-girdle amputation for five years (3-15-31). In considering the chondromatous type, we must be very sure that we are not dealing with the epiphyseal chondromatous type of giant cell tumor, or benign or borderline osteogenic tumors. If the nine cases of epiphyseal chondromatous type were included as sarcomas, the prognosis would be much better.
Osteogenic sarcomas of the shaft may possibly have a better prognosis, for case No. 156 had a huge sarcoma and is well eight years after amputation. This case had prolonged radium treatment at the Memorial Hospital of New York prior to amputation. It was a very large tumor of telangiectatic type. We also have full data of another case, No. 147, well nine years after amputation, registered by Dr. C. C. Simmons. Registry No. 1016 is a recent case.
Osteogenic sarcoma in the lower end of the humerus. Case No. 299 was one of sarcoma occurring in Paget's disease and could not be traced. The patient is undoubtedly dead. Case No. 357, registered by Memorial Hospital Clinic of New York, was reported to be well three years after amputation, and since then could not be traced. No X-ray was registered.
All four cases of osteogenic sarcoma of the clavicle are dead. Three out of ten cases of osteogenic sarcoma of the scapula are still living. Case No. 759 was well four years after operation and radiation. Case No. 867 was a remarkable one which has survived ten years since excision of the blade of the scapula, followed by an attack of erysipelas. It is not supported by an X-ray, but there is unanimity of opinion among the pathologists on the fairly satisfactory slide.
Ewing's sarcoma in the humerus, as in other parts of the skeleton, appears to be more favorable in prognosis than osteogenic sarcoma. Case No. 246, reported by Bloodgood, was said to be well nine years after exploration and radium treatment, but the diagnosis is doubtful in my opinion. Case No. 326, registered by Meyerding of the Mayo Clinic, had survived eight years after amputation and radiation. In this case, the tumor had extended well into the upper end of the bone. Case No. 576, which was a tumor of the upper half of the humerus, treated by Coley with radium and toxins without amputation, was said to have been well six years after treatment. It is not supported by a microscopic examination, but the X-ray is very suggestive of a malignant tumor. It was complicated by a fracture.
That Ewing's sarcoma in the clavicle is sometimes amenable to excision, followed by radiation, is shown by case No. 28. This was registered by Dr. Andrew Hosmer of Salt Lake City, and was well supported by X-ray and microscopic evidence. A tumor of the outer end of the clavicle was resected with the whole outer half of the clavicle on March 28, 1919. The patient was reported to be well nine years later. This case was complicated by a small local recurrence about a year after the first operation. This was removed and postoperative radiation given.
Cases of Ewing's tumor of the scapula are also encouraging. Bloodgood has registered a case, No. 137, in which one of these tumors involved the whole spine of the scapula. A portion of the scapula was excised with the outer end of the clavicle in July, 1920, and in September, 1921, the remaining portion was excised. The patient was reported to be well about nine years after the second operation. This case was reported to Bloodgood by Dr. Buist of Charleston, S. C. The X-ray and slides are characteristic of this tumor.
Case No. 515 was a similar one, and was registered by Dr. H. E. Isaacs of New York with satisfactory data. The lower portion of the scapula was resected on March 28, 1923, and the patient was reported to be well in September, 1929, but to have died of pneumonia March 5, 1931.
Case No. 919 has not been heard from since operation.
The Atypical Sarcomas are also encouraging. Case No. 409, a large tumor of the upper end of the humerus, resembling a giant cell tumor in the X-ray, was treated conservatively after a biopsy. The patient was given toxins and radium by Dr. Coley, and later consolidation and bone formation took place in the tumor. She was reported to be well eight years later. The microscopic slide is poor and the pathologists cannot make a diagnosis from it. While the case is obscure, it is encouraging, for the tumor was certainly large and one would have given a bad prognosis. Cases No. 421 and No. 998 have not been traced. Case No. 83, a very large malignant tumor of the whole shaft and upper end of the humerus, was registered by Dr. Simmons. The patient is reported well nine years after amputation, although from the slide and from the X-ray a very bad prognosis would have been given. Although the data are well registered, there is no unanimity of pathologic opinion. Connor has included it in his series of Ewing's tumors, but others consider it an angiosarcoma. A somewhat similar case has also been registered by Dr. Simmons, No. 564, involving the lower end of the humerus and also much of the shaft. The data are also good but confusing. The case was reported well six years after amputation, but a year later there was a recurrence in the axilla, which was excised. While both cases are atypical, they were very large tumors, very invasive and histologically very malignant.
The one atypical sarcoma of the clavicle, No. 1059, is living three and a half years after excision.
The two surviving cases of atypical sarcoma of the body oi the scapula were probably as near to our former definition of periosteal fibro-sarcoma as any cases we have had. No. 447 was registered by the Presbyterian Hospital of New York and was reported well, except for tuberculosis of the lungs, eight years after partial excision of the scapula. Case No. Ill, registered by Bloodgood, was reported as well nine years after excision of a similar tumor.
No. 147 No. 156 No. 812 No. 867 No. 28 No. 137 No. 246 No. 326 No. 576
There are probably many surgeons who feel discouraged about our progress in the treatment of bone sarcoma. I hope they will feel somewhat more optimistic, for I do after making this study. Hope in prognosis may be emphasized again by calling attention to the following cases of five-year cures among primary malignant tumors of the shoulder bones.
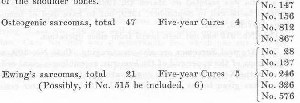
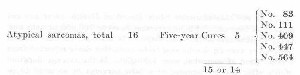
To find fourteen or fifteen living over five years out of eighty-four cases is certainly encouraging, and if we omit the twenty-four cases of osteogenic sarcoma of the upper end of the humerus, thirteen or fourteen out of sixty! Or, if we include the nine living cases of epiphyseal giant cell tumors, which some pathologists believe are sarcomas, we find ninety-three cases of sarcoma with twenty-three or twenty-four five-year cures. In my opinion this last should not be done.
THE RELATION OF TRAUMA TO BONE SARCOMA
The American College of Surgeons has widely advertised the Registry of Bone Sarcoma and has made repeated appeals to surgeons, rontgenologists and pathologists to register their records of instances of this disease. This propaganda has continued over ten years, and some $20,000 has been spent. Yet only 1,335 cases have been collected and studied. Only 655 of these are true osteogenic sarcomas. The Laboratory of Surgical Pathology at Johns Hopkins, together with Dr. Bloodgood's personal collection, had at their latest report only about 400 case histories of osteogenic sarcoma after more than thirty years. Coley, after forty years of the most arduous polemics in favor of his toxins and yearly papers before scientific societies as propaganda, has probably seen more cases than any other surgeon in the world. Yet, in a recent paper, he states that the combined records of the Hospital for Ruptured and Crippled and of the Memorial Hospital since 1890 show 855 cases. This included all forms diagnosed as bone sarcoma, and perhaps many were not sarcoma at all. Greenough, Simmons and Harmer found that in the Massachusetts General Hospital in a ten-year period, there were only twenty-seven cases of osteogenic sarcoma, although many other cases had been erroneously diagnosed as such. Since many of the cases of Bloodgood, Coley, Greenough, et al., are among those registered, the total number is not great. In 1922 from a postal card canvass of the doctors in Massachusetts it was estimated that at any one time there were not more than one of these cases in 100,000 of the population alive in this state.
According to the best information at present available (March,1933) at the Massachusetts State Board of Health, there are not more than four cases of bone sarcomas in every 100,000 persons now living in Massachusetts. This estimate is based on the fact that in 1932 there were 58 deaths said to be from this cause reported from a population of somewhat over 4,200,000. If the average duration of life after the development of a bone sarcoma be assumed to be three years, we may estimate that at any one time there are about 3 x 58 = 174 persons in the state who have this disease. This is likely to be a maximum estimate because we may be confident that some of these 58 cases were probably erroneously diagnosed bone metastases from cancer, so that the real figure is somewhere between that arrived at by my postal card canvass and this one from the Board of Health statistics; i.e., between one and four per every 100,000 of population.
These figures show that either the profession is excessively remiss in consulting experts on this disease and in recording their cases, or that the disease is an extremely rare one, notwithstanding the immense literature which has grown up about it. Yet the courts continue to give credence to expert testimony that in particular cases particular traumas cause particular bone sarcomas. How can any expert be justified in such statements when the disease is so rare? Trauma is an everyday event to normal boys and girls, and to many adults. Consider the frequency of traumas compared to the frequency of bone sarcoma.
How severe must a trauma be to act as a potential cause for one of these tumors? Theoretically, as a minimum, only of sufficient degree to stimulate the process of repair, and from that point up to a complete fracture of the bone. Certainly it does not vary directly as to the degree oi injury, because thousands and thousands of people fracture their bones and it is almost unknown to have a sarcoma develop at once at the site of fracture. Moreover, many cases are recorded where an X-ray taken immediately after the injury has shown signs of a sarcoma already at the site of fracture. The degree of trauma sufficient to make an ordinary black and blue spot, which necessarily causes discoloration of tissue and bleeding beneath the skin, would surely be sufficient to start the process of repair. We may, therefore, accept an ordinary bruise as a trauma of sufficient degree to initiate the repair process, which, either lacking a normal check or becoming unduly stimulated, runs wild and might become a sarcoma. What is the relative frequency of black and blue spots to sarcoma in 100,000 individuals? I think any mother or father who has noticed these spots on their children, even if only on Saturday nights during the few years that the bath is given and not taken, would agree that 10,000 bruises in a lifetime would not be an excessive estimate for each individual.
There is an impression among some doctors that bone tumors are much more common than I have estimated. I believe it is a false impression, although I will admit that many cases are never registered for two main reasons. First, these patients are notoriously difficult to diagnose and to cure. They usually go to several doctors before the diagnosis is made, and several more in hope of a promise of successful treatment, before death occurs. They often go from hospital to hospital. Second, being rare and spectacular cases, they are usually demonstrated at the Clinics as "interesting cases," and most of the doctors at every hospital see every case. Since each case requires the service of the X-ray Department, of the Pathologic Department and of the Surgical Department, the members of each service have the case impressed on their memory. The pathetic character of these cases, which are usually in strong young people and yet rapidly fatal, also makes them memorable.
I think enough has been said to show that these cases are rare, and I feel that I am conservative in saying that one case in 100,000 persons is a maximum estimate. If every person has 10,000 bruises, 100,000 persons would produce one billion combinations of person and bruise, to only one bone sarcoma. This seems a difficult argument to combat for those who wish to show that a given trauma caused a given case of sarcoma. You must turn your mind away from mathematics and think from a human nature point of view to get the idea that a certain trauma caused a given case of sarcoma.
It was your boy who had the bump which was followed two months later by the tumor. You find that one of your friends has a friend whose boy had sarcoma preceded by a bump. You become more convinced that bumps cause sarcoma. One of your neighbors heard of a boy who had this trouble and he recovered damages because the bump was received while the boy was at work. Your lawyer confirms this and adds that many such cases have received compensation for such injuries. You become more convinced that the bump in your boy's case caused the sarcoma. You feel sure he had no sarcoma until he had the bump. Your lawyer tells you that famous medical experts have testified that a large percentage of all cases of bone sarcoma had bumps within a year prior to the time the sarcoma was noticed. These experts have testified that they believe bumps cause sarcoma, even if they will not say that the particular bump in question caused the particular sarcoma. And some will even swear to that. By this time you are convinced that if your boy is not awarded compensation a great injustice will have been done. And furthermore, you will hear from your lawyer that insurance companies are generally ready to settle such cases out of Court, so great is the probability that Accident Boards and jurors will decide in favor of the poor boy with an amputated leg or arm.
At this point, the argument that 100,000 boys each bump themselves 10,000 times without having sarcoma, will go in one of your ears and out the other. You will say that 10,000 aviators might each fly 100,000 miles, yet one bump might kill any one of them, and think you have drawn a parallel. But the two propositions are not parallel and are widely different. It would be as logical to say that if one aviator in 100,000 had a bone sarcoma, aviation causes sarcoma. If all the aviators bumped in every mile the parallel would be more reasonable, for aviation would stop, and so would the human race if trauma caused sarcoma.
Suppose that your boy had a very slight prominence on his shin. You happened to notice this slight prominence. There is a beginning to everything. From your experience in counting the black and blue spots on his shins, how long will it take him to get one on that particular lump? Not long, you must admit. Then you and he will notice the lump and observe that unlike the other spots this lump will not go away ^altogether. In a month or two it may enlarge still more and become painful, and prove to be a sarcoma. Which black and blue spot caused the sarcoma? One of those previous bruises you have seen in the last five years, or the one that came after you had already noticed the lump? You will have to admit that if you have a boil or a bruise on some part of your person, some friend downtown is sure to hit it. How often has your other boy, who has no sarcoma, complained that when you grabbed him you hurt his sore arm or sore leg? Confess that you are too busy to count the lumps and black and blue spots on your boy every evening. Yet you say you are convinced that this particular bump caused this particular lump, and your lawyer thinks so, too. I admit that you may find the jury sympathetic and ready to be convinced. When the experts take the stand and swear they believe bumps are contributory causes of bone sarcoma, very likely you will get a verdict. Yet personally, I think the chance of any one boy getting a bump on a particular sarcoma is much greater than the billion to one chance of any particular bruise causing a sarcoma in 100,000 boys.
Let us see what grounds any experts have for such a statement as that sarcomas are caused by trauma. I will ask the questions and answer them as truthfully as I can, even though I favor the billion to one idea. I will now appear for the plaintiff.
Question. Do you believe that a blow or a bump may be a cause of a bone sarcoma? (Notice wording is not may cause.)
Answer. Yes. (Sotto voce explanation to my conscience.) Maybe a contributory cause.
Question. Why ?
Answer. First, because a high percentage of these cases give a history of a local trauma preceding the discovery of the tHmor by a number of months, and such a trauma may be assumed in the others. (This is entirely to impress the jury, because it does not impress me a bit, although I cannot be called a liar for saying it.) Second, because certain doctors, experimenting with malignant tumors in animals, found that when tumor cells were injected into the blood of these animals, tumors developed at places in the parts of the bodies of the animals which were purposely traumatized. (Also impressive but quite illogical.) Third, because the structure and the microscopic appearance of bone sarcomas vaguely resemble the process of repair which takes place when a bone is broken. (The only reason that I personally have any respect for.)
Question. Any other reasons?
Answer. Yes. (Followed by some learned "hot air," which is of no real importance.)
Question. Do you believe that the particular trauma caused this particular tumor?
Answer. It may have. If the patient had such a trauma as he claims it may have caused the tumor. (Drawing a red herring across the trail by focussing attention on whether or not he had the trauma.) (It may have—one chance in a billion!)
Now I will appear, for the defence and answer the same questions.
Question. Do you believe that a blow or a bump may be a cause of a bone sarcoma?
Answer. Do I understand you to say cause or be a cause? I do not believe that sarcomas are caused by blows.
Question. Why?
Answer. Billion to one argument. Disease far too rare, etc.
Question. Do you believe that the particular trauma caused this particular tumor?
Answer. No—not a chance in a thousand.
I am not a very popular expert, for these are about the extreme limits to which I could force my conscience. Fortunately for these pathetic patients, there are experts whose minds work differently.
I have come to the conclusion that there are two kinds of minds, each of which may honestly answer the same question in diametrically opposite terms, although the same facts are known to each intellect. One kind of mind will say that because the ratio of occurrence of bone sarcoma to trauma is one in one billion, it is folly to attribute a given case of sarcoma to a given trauma. The other kind of mind will conclude that although the ratio of sarcoma to trauma may be only one in a billion, if, in a thousand cases of sarcoma there was history of trauma in every one, it would prove that sarcoma was caused by trauma. Now, the first kind of mind might admit on purely theoretical grounds that sarcoma may be caused by trauma, and yet deny that one could associate any particular sarcoma to any particular trauma. Number two mind might disregard all theory in the matter, and simply assert that because every one of the thousand cases which he had ever heard of followed trauma, sarcoma must be caused by trauma. As a matter of fact less than one-half of the cases give a history of trauma.
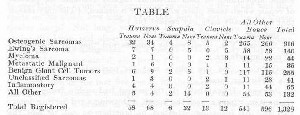
It seems to me we can make the subject a little plainer by comparing it with the condition known as hemophilia. Hemophilia is a hereditary condition, characterized by the absence of the ferment in the blood which normally causes clotting. These patients sometimes bleed to death from a trivial cut, from a nosebleed, or from the socket from which a tooth has been pulled. Hemophilia probably occurs in about the same frequency as bone sarcoma. A cut never causes hemophilia. The condition is there from the time of the birth of the individual. One particular minor cut may cause the patient's death in the ordinary, everyday sense of "cause." If the patient bleeds to death from that particular cut, was not the cut the cause? One may say normal persons do not bleed to death from such a cut; it was this condition, hemophilia, which was the cause of death. Now hemophilia differs from bone sarcoma in at least one very important respect, although the two conditions are comparable in the way I have stated above. In the case of bone sarcoma, the supposition is that there may be a control lacking, comparable to the absence of the fibrin ferment, so that the patient repairs to death, just as the hemophilia patient bleeds to death, in consequence of the trauma. The difference is that in hemophilia, any particular cut may be definitely associated with the trauma, for the condition, hemophilia, is well understood, while the condition, bone sarcoma, is still unexplained. We merely guess that it is a result of repair which goes on unchecked. There is no definite proof that this disease is due to the lack of normal repair check. It is merely the most plausible theory yet offered. There are many other theories, some of which would be entirely incompatible with a trauma being the cause of the onset.
If it is just that damages should be paid for a patient with hemophilia who bleeds to death from a trivial cut, it would seem to me fair enough, although by no means so definite a matter, to compensate a patient with bone sarcoma, provided it could be shown that there was a reasonable relation of elapsed time between the injury and the first positive X-ray. Such a decision could not be given because there was as clear a relation as in the case of hemophilia, but because it is desired to give the benefit of the doubt to the unfortunate person who was the sufferer. Practically, I do not believe that one case in a thousand of bone sarcoma is caused by the particular trauma to which the patient attributes it. From experience with little injuries of my own, those of my family and of my personal friends, and of many patients, I know that any sore spot will soon be bumped and that many a sore spot is not noticed until it is bumped. It is far easier for me to believe that the average person would be ignorant of a lump on one of his bones until it was bumped and then notice it for the first time, than it would be for me to believe that any one of the thousands of bumps that a normal person receives in a lifetime could in itself cause a tumor. There is very much less evidence of a relationship between trauma and bone sarcoma than there is between hemophilia and trauma. Trauma may cause death in a patient with hemophilia by starting bleeding which may not stop. It is hypothetical to suppose that trauma may cause death in a patient who lacks the normal check to repair, and therefore repairs to death with a bone sarcoma.
Whichever kind of mind is right about trauma being an exciting cause, there is some reason to believe that a trauma may disseminate the disease and make it worse. It might, for instance, break the fibrous capsule limiting the tumor and allow the cells to get into the veins and hence to the lungs. But in nearly all bone sarcomas this happens within a few years, at any rate. It has never been shown that those cases with traumatic histories die sooner than other cases, but it seems probable that they may. Nearly all these cases die within two years from the time when the tumor is first noticed. In other words, every one is always receiving bumps. The Registry will have to collect many more cases before an intelligent opinion can be formed as to how much a blow decreases the chances of a patient with bone sarcoma. This question is intimately bound up with the question of how much chance there is of spreading the disease by an exploratory incision, or by spontaneous fracture.
The Registry Committee, after thirteen years of effort, has collected only sixty-three cases of five-year cures of osteogenic sarcoma (all bones included), in which the diagnosis could be considered as even moderately well substantiated. Of the sixty-three, at least twenty-three had had exploratory operations prior to amputation. An exploratory operation is certainly as likely to spread the disease as is any other trauma. Since most cases of bone sarcoma, with few exceptions, die within five years, and since a large percentage of these few exceptions are known to have had exploratory operations, pathologic fracture or other trauma, it may be seen that an expert opinion stating that a certain trauma spread the disease in any individual case and hastened the patient's death, would rest on frail evidence.
There are other reasons, which we may briefly mention, leading to the conclusion that it is unlikely that trauma is an important factor in the causation of bone sarcoma.
If trauma were a cause we might expect the bones most often traumatized to show the highest proportion of malignant conditions. This is not the case, for every one interested in these questions knows that the phalanges of the fingers and toes are rarely, if ever, affected by sarcoma, yet they are the most common seats of trauma. The middle of the shin bone, which is very often traumatized, is not a frequent seat of the disease, nor is the skull. Many of the parts commonly affected are in positions where the bone is shielded from trauma by large muscles.
On the other hand, it is well known that these lesions most commonly occur near the ends of the bones toward which the nutrient arteries point. The Registry statistics unequivocally support this statement, which cannot easily be reconciled with the traumatic theory.
Cases of metastatic lesions from cancer, which occur in the bones, give histories of preceding trauma almost as frequently as do those who have primary sarcoma, yet no one even pretends to believe that metastatic lesions are caused by trauma; located possibly, but never caused.
The table of registered cases shows the proportion giving traumatic histories under the different diagnoses. The number having a history of trauma is unduly large, because, in both the primary and secondary lesions, every possible history of trauma is included, even if, as in some cases, a pathologic fracture was the first symptom. Thus, in only a minority of these cases, even if we accepted the largest possible figure, could the trauma have a causative relation with the tumor, so that the proponents of trauma as a cause would have a very poor argument. To my mind the large percentage giving a history of no trauma is of more significance than the large percentage alleging possible trauma. In fact, if all recorded cases gave a history of trauma, I should still think that judgment was in favor of the billion to one argument, and that the burden of proof as to causative relation still remained with those who held that such a relation existed.
REFERENCES
The Registry of Bone Sarcoma of the American College of Surgeons at 40 East Erie St., Chicago, maintains an up-to-date bibliography of the subjects considered in this chapter.
It seems to me that Kolodny's book, which is in fact an official publication of the Registry and which may be obtained from the American College of Surgeons, 40 East Erie Street, Chicago, 111., covers the subject of malignant bone tumors in general, better than any other publication which has come to my attention. I regard it as unfortunate for progress in knowledge of this subject, that Geschickter and Copeland in a more recent book (published by the American Society for the Control of Cancer, 1932) have taken the responsibility of making radical changes in the classification which has been offered by the Registry as a standard. If the authors had registered cases illustrative of their new nomenclature, or better still had re-classified the Registry cases with publication of the Registry numbers, their book would have been more instructive to the members of the committee and to future students. However, the book is evidence of a great deal of painstaking study, and I am sure that the other members of the committee feel as I do that it deserves praise and not blame, even though it seems to ignore the nomenclature at which we had unanimously arrived after days of discussion. We welcome any addition to the world's knowledge concerning malignant tumors of bone, but we would like to have illustrative cases of new entities registered as examples, or to have our attention directed to specific instances of our errors in classifying our old cases. We know that the future will show in many of our cases that our opinions, written before the final result in each case was known, will prove to be wrong. That is a part of the game we undertook to play. Changing the rules during the game, on mere authority without registered example, seems a little childish.
,



