Calcified deposits in the supraspinatus tendon
CHAPTER VI
As far as I know, the first patient to be operated upon for this -condition was Miss McM., age 24, Massachusetts General Hospital, No. 127430, June, 1902. I assisted Dr. F. B. Harrington to incise and drain what we took to be an abscess of the subacromial bursa. A culture of staphylococcus aureus was obtained, but the wound showed no sign of infection and promptly healed. I believe now that the culture was contaminated, for I have never been able to obtain a culture from one of these cases since. On reading the record now the description seems impossibly stupid, for in spite of the fact that I was even then interested in the anatomy of the bursa, and also had been an enthusiastic pioneer in using the X-ray for six years, I did not put two and two together and realize that the condition was what we now call a "calcified deposit." It was not until May 17, 1905, when Dr. C. F. Painter asked me to see with him another doctor who was in such acute pain that he begged to be operated upon, that we suddenly understood almost as much as we know now about the condition. Yet I think that even then we were the first surgeons to realize what these cases were and how easy it was to relieve them.
I mention these experiences to illustrate how blind the human mind may be to facts which are perfectly obvious, and when such facts are clearly demonstrated how difficult it is to diffuse them so that they may be generally applied. Rontgen's discovery had for several years made the lesson we learned from this case plain for any surgeon to read, yet no one had seen it in just the right light. Those who happened to know about the anatomy of the bursa may not have happened to be able to read the X-ray, or to have had an appropriate patient, who, like our friend Dr. D., urged us to "try anyway." We tried and relieved him at once, yet today right in this city there are probably patients with the same condition being treated week after week as "neuritis." Dr. Painter and I have both written about our experience; other surgeons have confirmed what we say; we have continued to get excellent results from this operation; yet twenty-seven years have elapsed and some cases are still treated without even the diagnosis being made or the X-ray even used. Dr. Painter has reported this case in his original article, March 21, 1907; I also reported it in my paper published June 9, 1908, as follows:
"The patient, Dr. D , is a man of 37 years of age, of heavy (200 pounds) physique and plethoric constitution. His previous history is unimportant, except that ten years ago after playing baseball all one summer he used to have a great deal of pain and soreness in his right shoulder joint. Since that time he has had at intervals a great deal of pain and tenderness in the joint. The pain bothered him particularly at night and was at times severe enough to prevent his sleeping well. He stated that until within a few days he had been able to move his arm without any trouble in all directions; for instance, behind his neck, behind his back, and over his head, without especial pain. There have been times, however, when it was difficult for him to raise the hand over his head, but when it was once put in this position it was comfortable for a time. He used to occasionally put it in this position at night; after lying with the hand behind his head for some time, he would then put it down by his side again. In doing this there was always pain during the motion. He recalls at times having his wife wake him just as he was going to sleep with his hand behind his head and tell him to put it down by his side, so that he would not go to sleep in that position and find it stiff on waking. External and internal rotation of the arm could be gone through without giving any trouble whatever.
Eight days ago while in New York he suddenly noticed that the point of his shoulder was tender and painful and that the motions were much restricted. He could with difficulty get into his clothes, but could not reach his hip pocket as he had been accustomed to. During these days the soreness had persisted and there had been great pain, sufficient to prevent sleep at night and to require large doses of morphine; the only comfortable position was sitting with the elbow supported. The pain was so great as to make him desire immediate operation.
Examination showed that the external and internal rotation of the humerus on its long axis is restricted about one-half the normal arc. Abduction or elevation of the arm is impossible on account of the pain caused in the neighborhood of the greater tuberosity. Attempts at passive elevation of the arm showed that the scapula moves in conjunction with the humerus.
An X-ray from the posterior view shows a pyramidal shadow in the region of the subacromial bursa just above the greater tuberosity and external to the tip of the acromion, the base of the mass being downward and about an inch in length. Between the base and the greater tuberosity is a translucent band about a quarter of an inch wide, occupying the position normally occupied by the tendon of the supraspinatus. The mass is apparently in such a position that the tuberosity could not ride under the acromion without compressing it.
Operation, by Dr. C. F. Painter, May 17, 1905.
Under the impression that the mass shown in the X-ray was caused by a calcification either of the bursa or its base, a vertical incision of about two inches in length was made through the skin and between the fibers of the deltoid on the point of the shoulder over the greater tuberosity. When the fascia beneath the deltoid was reached a small opening was made in the subdeltoid bursa, and this was enlarged with scissors to an extent great enough to admit the forefinger. The aspect of the bursa was not abnormal inside except for some firm adhesions anteriorly which made it difficult to separate the plane of the bursa from the neighborhood of the bicipital groove and the anterior part of the greater tuberosity. With the finger in the opening, it was found that during the rotation of the humerus, a mass corresponding to the shadow seen in the X-ray could be felt to pass beneath the finger. This mass evidently lay at the base of the bursa on the top of the greater tuberosity. An incision was made into it permitting the escape of about half a drachm of sebaceous material resembling the contents of a dermoid cyst. The cavity, which resembled a wen or dermoid, was thoroughly curetted and the walls excised. The base of it was evidently the tuberosity and tendon of the supraspinatus; the roof was the base of the bursa. When the sac had been entirely removed, it was found that the motion of the joint under ether was perfectly normal, rotation and abduction being easily performed. The incision in the bursa was not closed and the skin was drawn together with silkworm gut and the arm put in the ordinary sling position.
Remarks :
The point of particular interest in this case is the persistence of the function of rotation in spite of the limitation by abduction. It is obvious that the position of the cyst allowed rotation with comparative freedom, but that attempts at abduction would crowd the cyst between the greater tuberosity and the acromion process and caused pain and spasmodic rigidity of the joint. The acuteness of the symptoms within the last eight days is explained by an inflammatory condition in the cyst. The previous attacks were probably due also to the same cause. That this inflammation did not involve the bursa to any great extent is shown by the persistence of rotation. Since the bursa was not inflamed it would be readily seen that the symptoms which the patient complained of in regard to going to sleep with the arm behind his head can be explained, for the cyst having once got under the acromion was relieved of pressure. In other words, it was only when the cyst was inflamed by over exercise that its presence was noticeable, unless elevation of the arm crowded it between the acromion and the tuberosity.
The relief obtained by this operation was immediate and permanent.
It will be seen by comparing these notes with the description of the operation by Dr. Painter that the calcareous deposit seemed to me to lie not in the bursa, but beneath its base, and in or adjacent to the tendon of the supraspinatus."
It was difficult to find a heading for this chapter, and the one chosen is not satisfactory. An explanation of why it is not satisfactory may help the reader to understand the subject the caption is supposed to define. "Calcified subdeltoid bursitis" is a term in common use for the same condition, but this could not be accepted as a title for three reasons. First, the calcified deposits are rarely in the bursa, but lie beneath its base in the substance of the tendon of the supraspinatus or in one of the tendons of the other short rotators. To be sure, occasionally after inflammation has occurred the softened tissue containing a deposit bursts (See Plate II, Fig. 4) and the calcified particles are diffused throughout the bursa, the outlines of which may then be delineated by the X-ray. Fig. 44 shows an instance of this, but Figs. 45 and 46 are instances of the usual condition where the deposit is in its place of origin in the substance of the tendon, entirely beneath the base of the bursa. Therefore, "calcified subdeltoid bursitis" is a misnomer. It is also a wrong term because, as is explained on page 18, subacromial is a better term than subdeltoid. A third reason is the use of the word bursitis, as the noun which "calcified" is used to qualify. The bursitis is secondary to the pathologic process in the tendon. One may find no inflammation of the bursa and yet a large deposit beneath it may be demonstrated by the X-ray. It is only when the deposit is large enough, or the inflammation about it is great enough, to cause interference with the function of the bursa, that the symptoms of "bursitis" appear.
Our chosen title is also unsatisfactory because the offending deposit may not be in the supraspinatus tendon but in one of the other tendons underlying the base of the bursa, for instance, in that of the subscapularis. The infraspinatus and teres minor tendons may occasionally be involved. (See Figs. 45 and 46.) Sometimes two, three or even four tendons in the same patient are the seats of deposits. It seems to me highly probable that in most cases which show the deposit in one tendon there may be also a "tendinitis," or at any rate a degenerative change in the other tendons, which is not accompanied by much calcification, and therefore is not demonstrated by the X-ray. Furthermore, I am confident that I have seen instances in which the same tendinitis has produced bursitis by involving the base of the bursa before any calcification dense enough to be demonstrated has taken place. We might change the title to "Calcified and Uncalcified Changes in the Tendons of the Supra-spinatus, of the Subscapularis, of the Infraspinatus and of the Teres Minor; the Secondary Changes they may cause in the Subacromial Bursa overlying them, in some cases producing the Clinical Condition known as 'Subdeltoid Bursitis,' which should be called 'Subacromial Bursitis.'"
Even this extensive heading can be criticized, because there are still many cases never diagnosed as bursitis, but which pass as "neuritis." I might head the chapter "The Usual Cause of Neuritis in the Arm and Shoulder."
In 1908 I wrote as follows regarding subacromial bursitis: "The cases which are to be discussed in this paper are by far the most common lesions of the shoulder joint. It is the writer's experience that more patients seek hospital treatment for lesions involving the subacromial bursa than for all other lesions of the shoulder joint, including tuberculosis and fractures, added together." "Not only is this true, but it is also true that more cases of subacromial bursitis seek hospital treatment than all the cases of the supposedly more common forms of bursitis such as 'miner's elbow,' 'housemaid's knee,' and 'weaver's bottom.' In those clinics in which these statements are apparently not true it will be found that these cases are passing unrecognized under the diagnoses of brachial neuritis, periarthritis, muscular rheumatism, circumflex paralysis, contusion of the shoulder, fibrous ankylosis, gout, rheumatism and other vague terms."
These convictions have gained strength with the years, although I now wish that I had expressed them in better English. It may be almost taken for granted that cases diagnosed as neuritis, rheumatism, and arthritis of the shoulder, are really instances of subacromial bursitis; those with a distinct traumatic history being usually cases of bursitis due to rupture of the supraspinatus, and those of spontaneous origin being instances of the process I have tried to define above. Perhaps this seems a sweeping statement to the many physicians who still believe there is such a thing as brachial neuritis in otherwise healthy people; yet the statements are made in all sincerity by one who has studied the shoulder intensively for twenty-five years.
.jpg)
FIGURE 48. VARIED VIEWS OF A CALCIFIED DEPOSIT IN SUBSCAPULARIS
Tracings from three different films of a case in which a calcified deposit had formed in the subscapularis and had caused acute bursal symptoms. The deposit lying in the substance of the subscapularis tendon of course did not move about in relation to the lesser tuberosity; the apparent change of position is entirely due to changes in the relation of the bones in consequence of rotation of the humerus. The first film was taken in the anatomic position, and the deposit is overshadowed not only by the contours of the humerus but by the acromion. The second film was taken in internal rotation and the deposit appears to have moved over to the top of the glenoid. The third figure shows the deposit when the arm is akimbo; i.e., partly abducted and internally rotated. The deposit appears to have traveled to the lower edge of the glenoid.
This patient was operated upon by the writer, and the deposit removed. The incision was the same as in cases in which the deposit is in the supraspinatus; the affected area was just as readily brought under the incision by external rotation of the arm.
Deposits in the subscapularis are more frequently horizontal in their long axes than when they are in the other tendons. Compare Plate VI, Fig. 6. Sometimes they are not horizontal as in another case shown in d and e.
.jpg)
In order to make the condition plain the shadow of the deposit has been slightly intensified in these cuts. In the anatomic position (d) the deposit shows as a small speck internal to the bicipital groove, which in most antero-posterior X-rays can be located by the dense line of the outer edge of the lesser tuberosity. This line is an important landmark in X-ray interpretation, for by its position one may determine to a certain extent the degree of rotation of the humerus, and therefore make a reasonable guess at which facet shows on the contour of the greater tuberosity. Figure e is taken with the humerus held nearly horizontally and rotated inwardly as far as possible; i.e., the arm is in a high akimbo position. The deposit now shows in profile on the lower margin of the head of the humerus. Compare this plate with Figure 26, which shows an arm in the hammock position, in which the profile of the lesser tuberosity appears superior to the head of the bone.
The relation of trauma to the calcified cases is not yet clear. Since I first studied the subject I have always felt that it was highly probable that an acute or chronic injury to the tendon must occur long before the deposit appears. The pathologic histology of the lesion itself might be accounted for by faulty repair of an injury in tissue which has little vascularity and would be slow to restore itself. This was J. H. Wright's view from some tissue which I gave him. On the other hand, the fortuitous finding of the specimen shown in Plate VI, Fig. 5, indicates that the first change may be degeneration in the interstitial part of the tendon. Moschcowitz feels that the primary process is a tendinitis. Meyer, investigating from anatomic material, feels that both the biceps tendon and that of the supraspinatus may be attenuated from friction in overuse. I take issue with Meyer on the ground that I believe that destruction by friction per se does not occur in living tissue directly. Friction would first produce inflammation with resulting attenuation and atrophy of the part. I would expect in such tissue, if the local area became sufficiently poor in synovial lubrication, that congestion, tenderness and protective reflex spasm of the adjoining muscles would occur long before friction per se could do any damage. Whether the attrition be directly from friction or indirectly from atrophy following inflammation due to friction, the fact is that we rarely find ruptures of the supraspinatus in any but the aged laboring classes. The calcified cases on the contrary occur in young or middle-aged people, and moreover, they are usually not in people who do heavy laboring work, but in the more highly educated classes who do sedentary work, using the arms in a slightly abducted position for hours (See p. 135, Chap. V).
Since the calcified cases are, as a rule, in the middle-aged, and the rupture cases in persons at least elderly, some relation may exist. Perhaps aged cases in which rupture occurs had the tendinitis and calcified deposits in their earlier years, and thus had their tendons weakened and made prone to rupture. Or perhaps in youth strains which would rupture the tendons in older people result in merely the rupture of a few fibers. The capacity for repair is then great and restoration results. The same force in middle life might cause a slightly greater damage with hemorrhage into the tendon followed by faulty repair and calcification. Still later in life the same force might tear the aged tendon hopelessly. A partial parallel to this hypothesis is found at the knee, where the same kind of force in early youth avulses the tibial tubercle; in middle life the patella is the weakest point and gives way transversely, but in the aged the quadriceps extensor tendon yields in many cases. In other words, the relative tensile strength of the tissues has changed with age.
Although it is the rule that cases of calcified deposits recover with no known sequelae, I am more and more inclined to think that they must result in some atrophy of the tendon, whether they are absorbed naturally or are removed. I cannot believe that complete and sound repair takes place. This belief arises chiefly from a study of the microscopic changes which consist largely of a necrosis of the fibers. I incline to the belief that these same tendons may be prone to rupture in later years.
The Workman's Compensation laws (through the pertinent questions they put into the mouths of the members of Accident Boards and of Insurance lawyers) are sharpening the wits of modern Industrial surgeons in many ways and are having their effect on shoulder surgery also. As these little calcified deposits now cause loss to the insurance companies, they are assuming more importance than when they only bothered the individual patient. We are confronted with cases in which a slight trauma is alleged to have occurred and in which, after a lapse of a few days or weeks, disability has appeared and the X-ray shows the shadow of a deposit. Did the lesion precede the trauma? If so, did the accident aggravate the symptoms enough to make the difference between inability and ability to work? May the occupation which called for unusual or repeated use of the affected tendon have caused the lesion prior to the alleged accident? Since in cases not associated with accident at all the symptoms frequently come on suddenly, might not the association with a trivial accident be merely fortuitous?
The answers to these questions can be founded on so little in the way of statistics or demonstrable facts that they come into the realm of expert testimony and are matters of opinion only. I will try to set down my own opinions and what few reasons I have to support them.
Precedence of trauma or lesion (i.e., of a single definite trauma). Since in a general way we know that the process of calcification of dead or injured tissue requires a considerable time, it is pretty clear that the lapse of only a few days after the trauma before the X-ray was taken would indicate that the lesion had existed prior to the trauma. The same would probably be true a week or two after the trauma, but there would be increasing doubt as the interval progressed from weeks into months. I incline in general to think that the lesion precedes the trauma even when the X-ray is taken months later because (1) I have seen no instances where an early X-ray showed no deposit and yet a later film demonstrated one. (2) Because I have seen many cases where the X-ray did show a deposit soon after the trauma. In other words, in my experience the calcification usually preceded the trauma and I have never been able to satisfy myself in any case that it followed the accident.
It not infrequently happens that the X-ray will show a quiescent deposit without any symptoms in the supposedly well shoulder, as well as in the traumatized one. In fact, bilateral deposits are so common as to make us doubt whether acute trauma is ever a cause. They suggest that the primary cause is a general one. For instance, a systemic one; an attitudinal one; a congenital morphologic one. Yet in persons who use to excess both arms in their daily work, a chronic traumatic cause might be postulated even in bilateral cases.
Aggravation by trauma. Any one who has seen the bursa opened at operation and beheld the angry, red tumefaction with its white or yellow summit would agree that a blow on the inflamed area or even a sudden excess of tension on the tendon might aggravate the condition. One can readily see that the softened area might burst and spread its contents into the bursa under such circumstances. And it is clear that a trauma need not be very severe to do this. Yet to have the deposit burst into the bursa is in my opinion nature's way of curing it (Fig. 34). The acute symptoms are often soon followed by complete and permanent relief!
Excessive use as a cause. I am inclined to believe that this is the most common contributory cause if not the primary one. There are many instances besides "writer's cramp" and "housemaid's knee" to support the statement that in our division of labor the abuse or overuse of particular organs or tissues results in pathologic changes. Millions of years of heredity have not prepared the modern stenographer or machine operator to keep their supraspinatus tendons stretched and under tension, on the qui vive hour after hour, day after day. While only a few individuals in these employments have a severe tendinitis or bursitis, I believe that could we see the supraspinatus tendons from a series of stenographers who have worked steadily five years or more, some pathologic change would be found in them. Miners do not all have "miner's elbow," but I venture to say that all those who habitually work on their elbows would show hypertrophic and degenerative changes in their olecranon bursas. It is therefore my opinion that when disability arises from these calcified deposits in industry, the presumption should be that they are "Industrial," unless it can be shown that the occupation is not of a nature to demand overuse in this region of the body, or that the patient at home pursues an avocation which causes such abuse. Nevertheless it would require many months or years of such abuse to produce a typical "calcified deposit," for the minute pathology of these lesions is of a chronic type, although the inflammation about them may be very acute.
Coincidence of onset with trauma. It is certainly true that many cases have a sudden onset of acute symptoms with no history of trauma. It is easy to suspect in any given case that trauma was only an afterthought to get compensation. I have suspected this was so in some cases, but in others there was a clear history of accident, leaving little room for doubt that the accident precipitated the symptoms. It seems to me that no rule can yet be formulated and each case must be decided on its own merits; the more vague the story, the less likelihood that the course of the trouble was influenced by the trauma. The character of the occupation, the condition of the other shoulder, the duration of the kind of work, and other circumstances should be taken into account. At present my tendency is to consider such cases as instances of coincidence, even when the symptoms followed soon after the accident and the X-ray was taken weeks later. It is so easy to hit any sore spot in the body and to attribute the soreness to the blow which drew attention to it! Add to this the incentive to obtain compensation and the psychologic fact that it is human nature to influence one's self into any belief in which one's fancied interest lies. Nevertheless I would not deny that a single trauma (if well proved and of sufficient force) could be the direct cause of the onset of disabling symptoms. Furthermore, in doubtful cases it is only just to remember that it is likely that the occupation itself may have been the underlying factor.
Symptoms. Symptoms may be absent entirely and yet the X-ray may show a large deposit. This fact is particularly striking in the bilateral cases, for one side may be symptomless and the other the cause of agony. Radiologists not infrequently find these symptomless deposits accidentally. Yet these facts do not prove that the disease may run its entire course without symptoms. On the contrary, since we often see a large deposit in a case which has had symptoms for only a day or two, it is clear that a symptomless case may at any time present symptoms. Therefore, we doubt whether any case ever runs its whole course without symptoms. Most of the bilateral cases I have seen had one symptomless shoulder at first, but perhaps a year or two later had typical symptoms come on in the other. I have yet to see a case in which a good-sized deposit disappeared without ever causing pain or restriction. Beyond question the X-ray demonstrates that spontaneous absorption takes place in most cases, although some such instances may be errors of X-ray interpretation. Some certainly discharge into the bursa and are absorbed from there. Whether there are actually cases which never give symptoms and run their whole course without complications, I do not know. Many never give severe symptoms.
Most cases run a subacute course, a few are exceedingly acute, and a few are truly chronic. An attempt to classify cases strictly in this way results in confusion, for we find many cases which are borderline and others which in their course pass through all three stages.
The usual history is not of acute pain at the beginning. The first symptom noticed is a slight, painful "hitch" during certain movements of the arm, such as in raising one's arm to put on a coat or in placing an object on a shelf. Sometimes reaching across a table for some object, as a pen or a salt cellar, causes this feeling. Women complain that they cannot do their hair. Little attention is paid to this until it becomes associated with every such motion. The slight pain becomes expected and eventually dreaded before such motions are performed, so that the patient corkscrews his arm in a peculiar way to avoid the "hitch." Instinctively he learns to rotate outwardly as he abducts and thus avoids pinching the inflamed point under the coraco-acromial ligament as the arm is raised. Presently the sensitiveness reaches such a point that involuntary scapulo-humeral spasm is produced, and the normal, smooth division of motion between the movement of the scapula on the chest wall and the elevation of the humerus on the scapula is destroyed.
Loss of Scapulo-humeral Rhythm.
Normally when one raises the arm to a position pointing straight toward the ceiling, much of the motion is performed by rotation and elevation of the scapula on the chest wall, while the remainder is performed by the true joint. (See Fig. 25.) The two motions go on pari passu, so that as one watches from behind it is impossible to say that either motion proceeds faster than the other. In nearly all affections of the joint or bursa, this even distribution of motion is destroyed, because the sensitive point, unwilling to move, sends its reflex telegram to the short rotators to lock the joint in a fixed position and to hold it there by spastic tension. This phenomenon is one of the most important for the student of shoulder conditions to learn, and its behavior in these cases of calcified deposit is very characteristic. At first it is not complete, the spasm being semi-voluntary in the sense that the individual can control the inhibition of it to a certain extent. For instance, in mild cases the spasm holds the joint fixed as the arm makes its upward journey for about ninety degrees. Then the individual semi-consciously relaxes it and the joint surfaces themselves carry out the remaining ninety degrees to complete elevation. When the sensitiveness is still greater, even a strong effort of will cannot relax the spasm and the arm only ascends so far as it can through the scapular motion—almost straight out from the shoulder laterally. Later the spasm holds continuously night and day until firm adhesions form, producing a fibrous ankylosis which effectually splints the inflamed parts until they heal. When healing has taken place the adhesions gradually stretch and motion of the joint slowly returns. The course of this whole process in the most severe case is about two years. The fixation is never permanent. The great majority of cases do not have this severe course. Probably none would unless delayed by injudicious treatment.
The cardinal symptoms of the whole picture are pain, spasm, limitation and atrophy. These four symptoms may make a variety of complexes according to their relative severity. In one case pain may be the predominant one; in another, spasm; in a third, adhesion. I have seen cases which ran an almost painless course as if the spasm was started at once without the sensation of pain being experienced. The painful stage when the spasm is intermittent or semi-voluntary was absent; spasm from the early days was complete and adhesions took place before pain was felt in any considerable amount. The ankylosis stage persisted for months, the patient's chief complaint being from the limitation of movement. Some cases have relatively little spasm, no adhesions and constant pain. As a rule the amount of pain is inverse to the amount of restriction. The physician may relieve the pain by fixation of the arm and allow the adhesions to occur at once, but as I shall show later this is bad practice, unless the patient is one who can afford to avoid using the arm for many months. In most cases the "hitch" stage persists for many weeks with gradually increasing pain until past the stage of semi-voluntary spasm when restriction dominates the picture.
Pseudo-neuritis. If there has been a long, painful stage all the adjoining nerves become sensitized and the phenomena we call "neuritis " supervene even when fixation has occurred. The pain or hyperesthesia, originally mainly felt in the circumflex distribution about the shoulder and near the insertion of the deltoid halfway down the arm, becomes more diffused. It shoots up into the neck, on to the back of the shoulder blade and down the distribution of the radial nerve to the thumb and forefinger. Even the ulnar and median nerves may become sensitized, the hand and fingers swell and the skin over them becomes glossy. The picture is that of "brachial neuritis," but removal of the calcified deposits relieves it!
When the patient has hugged this painful, tender, useless arm to his side for weeks it presents a most unnatural, misshapen appearance. The back of the hand and upper flexor region of the forearm are swollen, while the anterior portion of the wrist is not. The fingers are partially flexed and cannot be extended even passively. Meantime the sleepless nights, incessant pain, and the dread of incapacity and uselessness have had their dismal effect on the patient, who may reach a very pitiable condition. Drugs have only too often added to the unhappiness of the individual—the family has a querulous invalid to care for.
Fortunately this picture is not the usual one nor is it frequent at present in this community, for nowadays the X-ray is sought for most joint conditions and locates the deposit; the condition is treated more hopefully and intelligently than when the diagnosis of "neuritis" was more common. Mild cases are far more frequently seen today.
Pain at night and inability to get into a comfortable position is the most uniform and constant complaint in all stages of this disease whether in acute or chronic form. Even the adherent cases cannot sleep for long on the affected side. The average patient tells you that he could put up with the pain in the day if he could only get a good night's sleep. In the early stages before there is much spasm, relief may be obtained by sleeping with the hand behind the head. In this position the tender point lies beneath the acromion, where it has plenty of room and where the supraspinatus tendon is relaxed. It is probably the most favorable position for the blood supply to repair damages. Women seem to assume this position more readily than do men. If a patient told me that she had pain in doing her hair and could not get her arm comfortable at night without putting her hand behind her head, I should be pretty certain that she had a calcified deposit in her shoulder. If she added that there was pain in the lower fibers of the deltoid near its insertion in the humerus, I should feel still more certain. If I found a raised, tender point about the size of the tip of the finger on the greater tuberosity which moved as the humerus was rotated, I should consider the clinical diagnosis established, although subject to confirmation by the X-ray.
The location of pain in the region of the lower fibers of the deltoid six inches or so below the real lesion, is a curious but very constant phenomenon in these cases, in all stages of their course. The complaint of pain in this region is almost diagnostic without other symptoms. I am uncertain whether it is to be explained as reflex pain or as directly due to spasm of the lower deltoid fibers. If one compares the two arms by taking the lower parts of the deltoids between fingers and thumbs of both hands simultaneously, one finds a distinct thickening, and there is often tenderness, too, on the affected side, such as would be produced by a tonic spasm of the fibers. The pain located here may be subordinated in the acute cases to the local pain in the bursa. One can in acute cases mark out the exact limits of the inflamed bursa by carefully pressing with a pencil tip and obtaining the patient's cooperation in locating the line of transition to acute tenderness. This is a very definite line and it may sometimes be vaguely seen when the bursa is distended with fluid and fibrin. Even when the bursa is the maximum tender point, the lower deltoid region may be the seat of maximum pain. There may be no local tenderness over the bursa and yet much pain and some tenderness in the lower deltoid.
Acute cases are characterized not only by the above-mentioned, distinct, local tenderness, but by excessive spasm and pain on the slightest motion of the joint. An acute attack may at any time appear in the course of a subacute or chronic case, but the most severe attacks usually appear without warning or known cause, though sometimes following a slight trauma. They represent the onset of bursitis from extension of the inflammation about the deposit in the tendon beneath the bursa. The symptoms are those of an acute bursitis and are homologous with similar acute inflammations in other serous cavities, i.e., congestion, friction, pain, protective spasm, fibrinous exudate, adhesion, cicatrization, partial absorption. The acute stage is therefore brief, lasting a week or two. It is during this period when the bursa is full of fibrin that it may be outlined as described above. The patient may wake at night with agonizing pain in the shoulder and be unable to move the shoulder joint more than a few degrees. Tenderness over the bursa is exquisite. Spasm has fixed the joint rigidly so that the arm is held in the sling position and the patient cannot be persuaded to move it in the least. One can take the patient lightly by the thumb and he will follow submissively where he is led, his whole body on the alert to avoid using the joint in the slightest degree. He cannot by any possibility sleep on the affected side and usually tells you that since the pain began he has "walked the floor" or had to sit up in a chair. For several nights no ordinary remedies give relief and considerable doses of morphine may be required. Exploration of the bursa at this stage usually shows that it contains fluid and fibrinous exudate overlying the boillike elevation on its base with its crimson, turgid periphery and whitish center. Until one has seen this appearance it is hard to realize how much these patients suffer. It is in such cases that the relief by operation is particularly striking, but they often get well promptly without operation or any treatment at all.
.jpg)
FIGURE 44a. BURSA DISTENDED BY FLUID CONTAINING CALCIFIED PARTICLES (Natural size) Case 141
.jpg)
FIGUBE 44b. A DISTENDED BUBSA IS CONCAVO-CONVEX (Size reduced one-half)
a. Shows the greatest distention of the bursa which I have ever seen from this cause. The film was taken by Dr. A. W. George, who referred the patient to me. I have, however, seen many bursse as much distended as this, in cases of rupture of the supraspi-natus, where the constant influx of fluid from the joint during efforts at abduction has dilated the bursa. Notice the gravitation of most of the calcified material to the bottom of the sac, which is bilocular, and yet enough particles have clung to the lining to cause its outline to show in the film. Case 141.
b. Schematic drawing to show that a distended bursa is a concavo-convex cap beneath the deltoid and placed in an antero-lateral position over the insertions of the short rotators.
Such acute symptoms subside in one to two weeks, some cases being followed by adhesions of the bursal surfaces which last many months. More often, especially if the physician has not tried to help, the patient by binding up the arm, the spasm subsides, the soreness disappears, normal motion returns, the "hitch" reappears and the condition is the same or better than before the attack. There are various stages between these two extremes; in some cases the attack seems to clear up the whole trouble, but often more or less spasm and restriction remain for months. I am quite positive that in the cases which clear up, the soft material has perforated into the bursa and been absorbed there. In those cases which have been through an acute attack and on which I have operated long after, I have found the deposit drier and firmer and more crystalline in composition and more intimately combined with the fibers of the tendon than those operated on in the acute stage. The deposit is likely to be firmer in chronic cases which have never had an acute attack. Apparently in acute attacks invasion of leucocytes about the deposit produces a sterile pus which mixes with the finely divided calcareous matter and softens it to the consistency of cream or butter. This creates tension in the substance of the tendon and tends to make the softened matter point into the base of the bursa. For some unknown reason perforation does not occur into the joint. It is the inflammation of the synovial base of the bursa which produces the symptoms so suddenly and starts the sequence of friction, pain, spasm, exudate, etc. At operation one usually finds the softened material under tension, so that when the white or yellow head of the boil-like center is nicked with the knife the material is squeezed out, as if it had been pent up. The operation gives relief to the tension and is effective in the same manner as in opening a boil. It is an interesting fact that under local anaesthesia the patient may express relief as soon as the tension is lessened. It seems that in these acute cases there are two kinds of pain, a deep, severe ache due to tension in the tendon, and the friction pain of the inflamed bursa.
I hesitate to describe a chronic form of this condition, since I have seldom known of an instance of more than three years' duration. Nor do I know how long symptomless deposits may exist. What I mean when I speak of a chronic case is one which lasts many months without going through an acute or adherent or neuritic stage. A case in which throughout its course the symptoms are confined to the painful "hitch," pain in the lower deltoid and a distinct rotating sensitive point, I should call chronic. In such cases the amount of the deposit as shown in the X-ray is usually small, perhaps minute, or even not demonstrable. Probably many such patients never consult a doctor. I see them more often among my friends who tell me casually about their symptoms, having heard that I am "interested in shoulders." Patients who consult me and have X-ray proof of the diagnosis and are told that the deposits are no harm in themselves, and that no operation is necessary unless the pain is severe, seldom come back to report when they are well. So that I can only give my impression that mild chronic cases do exist and that their duration, like the subacute ones, is seldom more than three years. As this was being written a patient on whom I had operated for a severe acute attack in his right shoulder, nearly eleven years ago, called to see me about his left shoulder. The right had remained well. Reference to my old notes showed that X-rays had revealed a deposit in his left shoulder at that time. He had been conscious that the left shoulder was not well, but it gave him no real bother until about six weeks ago, when mild symptoms began. They are still mild and he is taking diathermy. X-rays show that there is no deposit at present and there is a slight roughening of the tuberosity at the facet of the supraspinatus tendon, but there is no such roughening on the right side, which was operated upon. Evidently in this case the left ran a truly chronic course without complications. This one case, so far as it goes, indicates that the ultimate damage to the tendon may be greater if the deposit is not removed.
Atrophy of the spinati is found in all cases which have had severe symptoms for more than a few weeks. I have observed it in acute cases as soon as three weeks after the onset, and it doubtless may occur even earlier than this. Looking at the patient from behind one sees the spine of the scapula on the affected side more distinctly. In adherent cases this appearance is very pronounced and the shrinkage of the muscles may be so great that complete paralysis is suggested. I am inclined to think that in the worst cases the muscular bellies are in a condition resembling that of the muscles of the forearm in Volkmann's paralysis, which in fact is an ischaemia. However, they regenerate better under appropriate treatment. In such cases I am satisfied that rough manipulation under ether may rupture the muscles themselves rather than the adhesions in the bursa and joint. Atrophy of the deltoid is also usual; I have known of cases being mistaken for circumflex paralysis. The biceps also is as a rule more or less weak, and in long-standing cases all the rest of the muscles of the arm show the result of lack of use. The teres group is usually found in spasm and it is difficult to tell the amount of atrophy, for they are contracted in contrast to the spinati which atrophy in a stretched position. When one stands back of the patient and with forefingers in the axillae and thumbs behind the posterior axillary folds, and one palpates the muscles near the border of the scapula, one finds that those of the affected side are thicker and firmer than those of the normal side. Nevertheless, there may be atrophy of these muscles. The fact is that the spastic teres muscles are shortened by adduction of the arm and thus appear thick on palpation. Yet they may be shrunken as a whole although short and thick from constant spasm. These spastic muscles are always somewhat tender. This thickening and local tenderness of the teres group should not mislead us, for the cause of their sensitiveness and spasm is. not local in these muscles.
In examining for shoulder lesions of any sort it is important to note the condition of the spinati. Atrophy of these muscles is an accompaniment of all lesions of the shoulder joint of a serious inflammatory nature. I do not find it in cases of malingering and of hysteria. Furthermore, its degree is a fair gauge of the gravity of the lesion, and also serves to gauge the prognosis.
It may be seen from what I have said about the symptoms caused by calcified deposits in the tendons, that a strict division of cases into acute, subacute and chronic cannot be made. I cannot take my own series and pile them in three groups of records after this manner. Neither can I separate them into adherent and non-adherent cases satisfactorily". Restriction of motion may be slight or complete and of all degrees between. Yet these divisions are all clinically useful, though ill-defined, and mean something, at least for a time, in individual cases. A corollary can be drawn from this that prognosis is uncertain. One cannot tell in a given case exactly what its course is to be. This makes advice as to treatment and comparison of results very difficult.
Restriction of motion is usually in one or both of two different arcs of motion, i.e., in external rotation and in elevation. When elevation is restricted and external rotation is free, one should suspect at once a condition in which the inflammation about the calcified deposit is great enough to make a mound in the base of the bursa, but has not yet created irritation of the synovial lining of the bursa. Rotation is painless because the inflamed, raised spot can rotate under the deltoid without striking any hard or any firm tissue. On the contrary, when abduction or elevation is performed, the inflamed mound is pinched between the tuberosity and the acromion or coraco-acromial ligament. The pain thus caused instantaneously produces scapulo-humeral spasm and the upward movement is restricted. Let this patient stoop over as far as possible with his shoulder muscles relaxed and the arm abducts on the body by gravity. The tender point rides easily under the acromion in this position because the supraspinatus is not acting to produce tension about the deposit, nor is the deltoid pulling the humerus vertically upward against the acromion. If the patient then fixes his shoulder voluntarily, he can stand upright with the arm elevated.
Such cases as I have just described can usually be separated from malingerers, because one can always find the rotating tender point where the deposit is, for it is easily felt as it passes beneath the deltoid fibers. Furthermore, having made the patient stand with the elevated arm, he will be seen to have a "hitch" or a period of scapulo-humeral spasm as he lowers it from the vertical position, and the tender point in its downward journey again passes the narrows under the acromion. This sign is also a sine qua non of complete rupture of the supraspinatus, but in the latter no calcified deposit is shown by the X-ray.
A symptom which is occasionally seen in these cases is what I call the "down-it-will-go" symptom. It is rather infrequently complained of, but often acknowledged if asked for. Patients with complete rupture also show it. A patient will say that the arm is paralyzed or that he is afraid it is going to be paralyzed. He reaches for some small object or is carrying one, and "down-it-will-go." It seems to be an involuntary sudden relaxation of the grasp. It frightens the patient, although it is usually spoken of diffidently or with an apologetic laugh. It is irregular in its occurrence. I cannot explain it, but my theory is that it is a phenomenon associated with position sense. I have already stated that in some cases spasm starts without pain. In a case of circumflex paralysis which I observed, and on which I operated under local anaesthesia to see whether the supraspinatus was torn, I found that the interior of the bursa and the joint were completely insensitive although the skin sensation was present. In a doctor on whom I was operating under local anaesthesia for a calcified deposit I could at will start spasm without pain by touching the base of the bursa. These observations indicate that the bursa and joint are supplied by nerves which do not transmit ordinary tactile pain but serve to excite the scapulo-humeral reflex. It may be that this "down-it-will-go" symptom is something caused by this set of nerves, when, in reaching for the object, the sensitive point comes against the acromion. Without consciousness the grasp relaxes in order to get rid of the weight which, by leverage, increases the pressure on the tender point. In this connection we also have the phenomenon that the pain in these cases is as a rule attributed to a point near the lower insertion of the deltoid.
.jpg)
FIGURE 45. CALCIFIED DEPOSIT IN THE TERES MINOR
In interpreting X-rays of calcined deposits one must be sure of the position in which the film is taken in order to say positively that the calcified material has escaped from a tendon into the bursa. This is particularly true in cases where the deposit is in the teres minor, as in this picture. The insertion of the teres is very low and if, as in this case, the view is taken with the head of the bone in inward rotation, the deposit appears to lie in the bursa, when in reality it is still confined within the tendon substance
.jpg)
FIGURE 46. CALCIFIED DEPOSIT IN THE INFRASPINATUS
Figure 46 was taken with the plate on top of the shoulder and the rays nearly parallel with the long axis of the humerus, in order to bring out the bicipital groove. The prominent deposit in this case was in the infraspinatus, as is shown by the fact that it is about one-half inch exterior to the bicipital groove. There is also some deposit in the supraspinatus which shows poorly in this picture, for it is overshadowed by the tuberosity.
There should be some differences between the symptoms of cases of deposit in the subscapularis and in the supraspinatus. The location of the tender point, whether inside or outside of the bicipital groove as shown by the maximum spot of tenderness, is my usual way of differentiating. Careful study of the X-ray is confirmatory. Whether the symptoms themselves differ I am not sure. One would think that external rotation would be limited in subscapularis cases, but I have not found this true enough to rely on. A recent quite acute case had no such limitation. Another case of bilateral subscapularis deposit which occurred in my own household had symptoms quite like those in a supraspinatus case except in the location of the tender spot. My series of cases is not large enough to make comparison, but the point is important because it helps in performing the operation.
The X-ray should confirm a diagnosis of calcified deposit, but one should be very exacting in demanding excellent technique and films made from several angles before making a negative diagnosis when the clinical picture is typical. This is particularly important in ruling out a deposit in the subscapularis tendon. A recent instance was only positively diagnosed by a fourth film which showed the deposit in profile. The deposit was large, but in the first three positions the shadow overlaid the bone in such a manner as to elude experienced eyes, although after the fourth film it could be identified in each picture. A very slight rotation of the humerus may throw the shadow over the bony outline, especially if, as often happens, there is only a mere fleck of calcareous material. Even a large recent deposit of little density is easily overlooked. The Rontgenologist must learn to take pains to get each facet of insertion in profile.
Even before calcareous material is demonstrated by the X-ray, the diagnosis on clinical signs alone may be made with a considerable degree of certainty.
Treatment.
Since the prognosis of these cases is always eventually a good one, and since in any given case the probable course cannot be foretold with certainty, no treatment of a dangerous nature can be considered. Even a risk of any permanent minor damage would be unwise. All cases, whether treated or not, in which I have known the late result, have recovered without permanent complications of any kind. Recovery is only a question of time. The object of treatment is purely one of the relief of symptoms. Any one who wishes may endure the whole course of the trouble without other treatment than palliative remedies such as occasional doses of aspirin or the application of an ice bag or a hot water bottle. Many acute cases following perforation recover in a few weeks. Some persons prefer to endure daily pain month after month rather than to submit to a minor operation or go to the trouble and expense of prolonged treatment by physiotherapy. My personal opinion is that surgical removal of the deposit is practically free from danger, sure to relieve the severe symptoms at once, and, in fact, that it generally will relieve all really troublesome symptoms within a few weeks. It is not a painful operation; it can be done with local anaesthesia; it requires only a few days of hospitalization, and there is very little postoperative pain as a rule. It seems to me that the patients whom I have followed through an acute attack suffer more in forty-eight hours than does a patient who has been operated upon in his whole convalescence. I have performed the operation on a number of doctors, who have previously had acute attacks, and they have been of the same opinion. Furthermore I have seen, in subacute and chronic cases, the constant neuritic type of pain with consequent loss of sleep, reduce patients to a very serious physical condition, the relief of which would justify a much more dangerous operation. It therefore seems to me that it is better to have the deposit, if large, removed as a routine, than to run the risk of either an acute attack or of severe chronic pain. It is quite reasonable for a patient to say, "But I may never have any severe pain, and then the operation will have been unnecessary." This is quite true and the answer is that there is little objection to waiting until the actual pain makes the prospect of operation more welcome. It would be hard to say for another individual how much annoyance and loss of sleep is equivalent to the operative pain and discomfort. Certainly pain sufficient to prevent work is enough to demand an operation of the trivial character of this one. Statistics as yet cannot show in a given case what the chances are that serious pain will ensue.
I think it is fair to say that the severe pain is relieved at once by the operation and that the patient may expect the return of full use of his shoulder in from three to six weeks, although he may feel twinges of pain in extreme positions of the arm for several months.
In general my attitude is: "If I had your trouble I would prefer operation as the best way to avoid pain and disability. You will get well anyway, but your total pain and discomfort is pretty sure to be worse and likely to be much worse, if you are not operated upon. I advise you, but I do not urge you, to have this deposit removed. There is no danger of your having a crippled arm or any permanent trouble, whether treated or untreated."
Many patients, on receiving this advice and reassurance that they will not lose the use of their arm, prefer to endure the pain, annoyance and discomfort. Others ask what other treatment there is apart from surgery. The answer is that aspirin and similar drugs will help them bear the pain, particularly at night. Morphine will relieve the pain, but its use for more than a few nights is of real danger, for the pain may last many months and a pitiable habit result. No drugs are known which will cause absorption of the deposit when taken internally. Since the deposit is deep in the tissues and covered by skin, fat, fascia, muscles and blood vessels, in which the blood is circulating, no local applications as ointments, linaments, iodine, etc., can reach the lesion and do good. The most that can be expected would be slight, temporary relief from counter irritation, such as is gained by hot or cold applications. Massage and manipulation and active or passive exercises might be harmful unless most judiciously performed. After the acute symptoms are gone these agents may be helpful in restoring motion if it has become restricted. Very acute cases are apt to be very brief cases, and their spontaneous recovery may be coincident with surgical or other therapy.
I know of no form of electrical treatment which might be expected to remove the lesion except diathermy. It is rational to hope that the use of this form of physiotherapy might help nature to absorb the deposit and resolve the exudate about it. It is held that diathermy heats living tissues through and through, and the effect of this heat on such deposits has been claimed to cause absorption. Since these deposits are naturally absorbed in varying periods, it is difficult to be sure that their disappearance under treatment by diathermy is not a coincidence. No attempt so far as I know has been made to check up a series of cases so treated with an untreated series. The same criticism applies to the results of surgical removal, but we know then, that the deposits, and symptoms as well, are removed. In some cases I have operated after the patient had been treated with a course of diathermy, and yet found a large deposit. In others so treated the X-ray has continued to show the deposit for some months after the symptoms were relieved. However, it makes little difference whether or not the deposit is removed, if the pain disappears. I have known of a few cases in which this has happened after a few weeks or months of treatment by diathermy. They were relatively mild cases. In others I have operated when diathermy failed to remove either deposit or pain. Furthermore, after perforation in the bursa has occurred the deposit absorbs spontaneously within a few weeks. Yet if a patient wishes some treatment other than operative, I advise diathermy. I do not use it in my own work for two reasons. First, being inexperienced with its use, I should fear the danger of burning the patient more than I would the danger of surgery. Second, I know that operation permanently cures; I have some faith that diathermy will assist the natural process of repair.
Dr. E. B. Mumford of Indianapolis, who is a prominent orthopedic surgeon, believes that diathermy is the treatment of choice (Jour. A. M. A., Vol. 97, No. 10, 1931, pp. 690-694). He gives details of his technique. "All of our cases became well by this conservative form of treatment and in all cases with a deposit shadow, the deposit either entirely disappeared or became much smaller in size and less dense in the X-ray. In none was surgery necessary. The average number of treatments was twenty-one, given daily for the first two weeks and then twice a week. Relief from pain was obtained in from three to ten days. The end result was complete restoration of function without pain. Ten cases have been checked at the end of one or more years and no recurrence noted."
I am far from denying that diathermy is effective. It is too bad that comparative tests of different forms of treatment cannot be made. One thing is greatly in favor of diathermy, and that is that it is necessary for a surgeon to know the anatomy and pathology of this particular region if he is to obtain uniformly excellent results by operating.
There is one form of treatment not uncommonly given, which I believe is to be heartily condemned, i.e., fixation by strapping or bandage. In my opinion many of these cases are made worse by this treatment, which encourages adhesion of the roof of the bursa to the inflamed tendon. All the periarticular structures become fixed, the muscles atrophy and become ischemic and contracted. Many months may pass before the joint moves again, although ultimately it always does become mobile. The neuritic symptoms are particularly troublesome in such cases, although sometimes the ankylosis is entirely painless and the patients are only inconvenienced by the restriction. Spontaneous scapulo-humeral spasm is a sufficient guard for the inflamed joint and we should neither add to it with straps and bandages nor fight it with forced motions. Active "swinging exercises," with the patient in a stooping position, should be used in most cases. When the patient stoops the strain is taken off the supraspinatus and it is far easier to move the joint. I regard it as very unwise, until the convalescence is well advanced, to allow the patient to exercise the arm in a standing position because this forces the supraspinatus to cooperate with the deltoid in supporting the weight of the arm. The pain caused by this at once starts scapulohumeral spasm and the joint ceases to move. It is better to let the patient stoop with the arm hanging relaxed. If the patient straightens up again as soon as spasm begins, he will in fact adduct the arm. In other words, when one stoops with the arm relaxed one abducts (elevates) the arm on the body; when one straightens up with the arm relaxed, one brings the arm into the anatomic position.
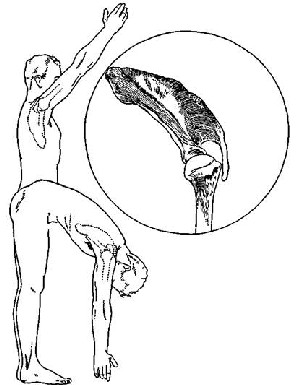
FIGURE 47. STOOPING EXERCISES
The principle of the stooping exercises is that they permit the patient to abduct the arm by gravity and therefore no fulcrum is needed. If a patient elevates the arm in the standing position, the humerus obviously must obtain a fulcrum on either the glenoid or on the acromion or on both, while in the stooping position no fulcrum is necessary. In the standing position the little supraspinatus must pull the tuberosity firmly to keep the latter from touching the acromion. In the stooping posture it may remain relaxed.
Since the sore point in most lame shoulders is on the tuberosity at just the region where it tends to obtain a fulcrum on the acromion, it is highly important that the patient with a damaged supraspinatus should not delay his recovery by frequently raising his arms. The exquisite tenderness which arises in these cases is nature's defensive effort to warn the patient not to use the arm in this way.
When the patient with the sore shoulder is in the stooping posture he can much more readily brush his hair, button the back of his collar or perform any other motions. He can, for instance, learn to put on his shirt and coat over the lame arm when stooping, and then after he has risen to the erect position put on the other sleeve.
When in the stooping position, either lateral or antero-posterior motions can be done with a pendulum-like movement without great muscular effort. In this position the humerus not only tends to avoid a fulcrum, but actually the weight of the arm helps to stretch the contracted tissue of the joint.
The principle of "stooping exercises" is useful in many ways. Gentle exercises of this kind prevent adhesions following the acute or subacute attack. Vigorous exercises loosen up adhesions already formed. Gentle postoperative exercises hasten convalescence; too vigorous ones start scapulo-humeral spasm and delay recovery. It is unwise to give passive exercise or permit active exercise which causes even moderate pain. Yet to fix the arm in bandages to relieve pain is also unwise. When one has seen the inside of these inflamed bursas one can readily understand the danger of either fixation or over exercise. Gentle motion, unhampered by bandages or spastic muscles, is indicated to prevent adhesions. The patient should be allowed to change the position of the arm as freely as he cares to. He should be instructed to keep it in external rotation as much as possible, because an arm held in the sling position is in internal rotation, and if it adheres in this position, it requires a long time to gain normal external rotation. We should avoid scapulo-humeral spasm not only because it promotes adhesions, but because much of the actual pain due to the spasm pressing the inflamed parts together. Spastic muscles are not only painful but tender.
In two early cases with very small deposits and mild symptoms I have tried the experiment of keeping the patient in bed with the arm abducted, in the way in which I treat cases in the non-calcified type. (See p. 218.) This treatment seemed desirable for several reasons. It is the natural position assumed by many patients to obtain ease; i.e., they sleep with the hand behind the head. In this position the supraspinatus is relaxed and its tendon is not stretched; this would permit an active blood supply to promote repair. This position would bring the inflamed portion of the tendon wholly under the acromion, where it could not adhere readily, and if it did adhere would tend to loosen from mere gravity. Both cases were soon relieved.
Another form of treatment remains to be mentioned—aspiration as suggested by Flint. After Flint's publication I tried this once with some success. I am satisfied that in this case I actually punctured the deposit and allowed it to leak into the bursa and thus relieved the pain. This was not exactly Flint's plan, but may also have been his achievement in his cases. I have opened so many bursas without finding much fluid that I doubt the wisdom of trying this procedure. Like most needling in other tissues, it seems to me to carry all of the disadvantages of an exploratory incision and some serious ones of its own. It would be rational to thrust a large aspirating needle into the deposit under guidance of the fluoroscope, but I would prefer to be operated upon were I the patient.
As in the case of many other ailments which affect the human body, there is great variation in the degree and duration of the pain it produces. Even very acute cases may recover completely in a few weeks with the simplest palliative treatment. Therefore any form of therapy is deceptive in its results. I have often had a patient postpone accepting my advice for operation and seen recovery promptly ensue! No surgeon should feel as did Jack Horner and say, "What a big boy am I!" after removing one of these deposits. These rapid cures occasionally occur after any of the other forms of therapy, for nature does the work in spite of what we do at the same time. Yet at the present date, I can unhesitatingly say that unless there is some good reason to the contrary I should advise operation in all painful cases, and in all cases where the deposit is as large as a lima bean, even if there is no pain. I sincerely believe that operation is a far less serious matter than fixation, and no more dangerous than diathermy or intravenous therapy.
END RESULTS IN CASES OP CALCIFIED DEPOSITS
The following study is based on an analysis of twenty-nine replies to a questionnaire recently sent to patients on whom I had operated for this condition long enough ago to indicate whether there have been any unpleasant after effects, due to the operation, recurrence of the lesion or other complications. The period elapsed since the operation was ten to twenty-four years in nine cases, five to ten years in eight cases, and one to five years in eleven cases. All these patients stated that they had had no further trouble of any kind with the shoulder which had been operated upon, but ten had had similar trouble of minor degree in the other shoulder. In most of these cases there had been evidence of deposits in the other shoulder at the time of operation.
These data confirm my impression that when these patients have been operated upon their symptoms do not return in the same shoulder. Furthermore I have not known of any late complication which followed about forty other similar operations on patients who did not reply to this particular inquiry.
Two patients whose deposits were in the subscapularis, will be given separate consideration later, and are not included in the following resume of the replies to the questionnaire. As in the case of most questionnaires, some of the answers were not satisfactory. For the sake of brevity, doubtful replies to individual questions will be omitted without making such notes as "answer equivocal," or "not stated." Consequently in the following analyses the sum of numbers in each statement will not always be twenty-nine.
Antecedent Trauma. Twelve stated that the attack followed a definite injury; thirteen stated that there had been no injury; three were uncertain. These figures are also in accord with my whole experience, which is that the injuries are usually trivial, and often uncertain. In compensation cases one is tempted to think that the history of injury may be purely an afterthought, although about half the cases may be said to give a definite enough history of trauma to account for rupture into the bursa. For instance, the twelve injuries were:
No. 79, business man, "Throwing baseball"; No. 81, iron worker, " Pulling on heavy bar"; No. 103, osteopath, "Fall"; No. 105, no occupation, "A bad fall down stone steps, and a sudden wrench later on"; No. 113, physician, "Fell on elbow with arm held rigidly against chest"; No. 121, surgeon, "Fall on stairs with violent swing of arms in attempt to preserve balance unsuccessfully"; No. 122, housework, "Wrenched shoulder in effort to avoid fall on staircase"; No. 138, osteopath, "Fall" ; No. 140, business man, "Fall from a horse"; No. 142, a business man, "In making motion of throwing spear felt a severe pain and was unable to raise the arm."; No. 143, waitress, "Raising tray."
The duration of symptoms prior to operation varied from a few days to ten years in one case. One man even stated twenty years, but the continuity was somewhat doubtful. There were eleven cases who stated that symptoms had existed from six months to five years, and two from one to six months. Ten were acute, that is, there had been no pain until within two weeks.
Relief of Pain. In acute cases pain was at once relieved by the operation and in chronic cases there was very little pain after the first few days. Eight patients reported no pain or actual relief from pain immediately after the operation. In other words, a really acute case is so much relieved by the incision that he may ignore the postoperative pain, but a chronic case, who has had no previous acute pain, is more aware of any later discomfort from the wound itself. Only seven mentioned pain after the first day and only one after the fourth day.
The subacute, annoying symptoms in convalescence varied from one to four weeks in most cases, but one case complained of some pain for seven weeks.
Use of Arm. Most patients began to use their arms within a few days and used them with more and more freedom from day to day. As a rule it took from one to three months before perfectly free use returned. By the end of three months all but two patients had ceased to be even annoyed by the shoulder. The symptoms of these two cleared up within seven months. One of these was an iron worker who continued to have pain on using a sledge hammer when he returned to work fourteen weeks after the operation.
Return to Work. In most cases the patients returned to work or to their regular avocations after a month or less, only three cases requiring more time, the longest being the above-mentioned iron worker. (An industrial case.)
Hospital Days. The time spent in bed averaged three and a half days. None were absolutely confined to bed. The time in the hospital averaged five and a half days; three patients remained only three hours; six remained ten days for convenience, not from necessity. All wounds united by first intention.
From the point of view of the operator, who does not endure the pain, the results of this study may be summarized as follows: In acute cases the severe pain is relieved at once by the operation, and even in chronic cases the postoperative pain lasts only a few days. Within a few weeks the patient is about his usual pursuits, although he still has transient pain in extreme motions and cannot lie comfortably on the operated side. Then follows a period of a few months during which certain motions may cause annoying, sharp, brief twinges, and at night the arm may still cause a minor amount of discomfort. These symptoms become less obvious, and presently days together pass without a thought of the shoulder. This period is indefinite, but is to be measured in months, not in years.
In order to get the patients' points of view I included in the questionnaire a request for a statement on their general impression about the efficacy of the operation. The following answers were given:
Case No. 51, a physician, "Operation entirely relieved my acute pain which had been present for several weeks. The other shoulder has been involved since, and has cleared up with no treatment. It was never as acute as the operated one"; Case No. 55, a physician, "... as I suffered so intensely for so many months and was entirely relieved within a few days after the operation. If you remember my operation was performed under local anaesthesia. My recovery was a very quick one and as nearly as I can remember I was able to do my regular work in a very short time. In April (2 and a half mos.) I was playing golf with no discomfort whatsoever"; Case No. 56 (from patient's physician), "I feel quite sure he thought it a success. Patient died of angina" (9 yrs. after op.) ; No. 62, "To me the desirability of the operation is unquestioned, in competent hands, however. The pain is so wearing and causes such nerve irritability that the sooner it is over the better. I consider my operation a great success, and would advise any one to put up with the temporary inconvenience"; No. 63, "Grand in every way"; No. 65, "Am pleased to say that I have no pain whatsoever and have perfect use of my arm; in fact, I have had since about two weeks after the operation"; No. 66, "I have never been quite able to make up my mind as to the efficacy of the operation. On the one hand I have had no discomfort in that shoulder; on the other hand, the ease with which I am able to control any kick up in the other shoulder by avoiding gouty foods and drinks leads me to believe that it might have been possible to cure it without an operation"; No. 68 (See Plate II, Fig. 8), "Extremely successful, has never bothered me since"; No. 72, a surgeon, "I obtained immediate relief at the time of operation and aside from some soreness of the wound, I was perfectly well, and as I remember it, I was operating within six or seven days of operation, the exact date I do not remember"; No. 73, "85-90% improvement" (This patient, a physician, had had symptoms for ten years) ; No. 79, "100% successful"; No. 81, "To secure any lasting benefit, I think that an operation is the only thing"; No. 85, "Similar to the removal of an aching tooth, pain all gone, only the soreness which would follow any deep gash in the body, would say no operation could be more efficacious"; No. 93, "Excellent"; No. 103, a physician, "Decided success"; No. 105, "Unqualified approval. The X-ray showed a quiescent bursa in the other shoulder. I have been a bit careful and when there has been the least twinge, have rested it. But even that has only happened three or four times in these years "; No. 113, a physician, "Absolutely perfect. The relief from pain and the conviction that there will be no recurrence are beyond price. Personally, I believe that any other procedure is a waste of time"; No. 114, "A wonderful operation. I walked home from the hospital three hours afterwards, and never had any pain or discomfort at any time except for a month when trying to use arm too strenuously. I recommend it heartily "; No. 121, a surgeon, " I was strong for it! At the end of one week I deliberately broke up adhesions by playing golf. After this the soreness subsided rapidly. The right shoulder bothered three months ago, no known trauma. Symptoms have now all subsided"; No. 122, "My impression is that the operation was very successful, and at times when my other shoulder troubles me I often wish I had both shoulders operated on"; No. 133, "Excellent results. I do not recall that I had any pain following my operation, with the exception of the few days I was in the hospital, and this was more from the soreness of the incision rather than actual pain from the shoulder. It was quite some time before I had the absolute free use of my arm, but I should say this was due to my lack of exercising it. However, it is absolutely perfect and I have used it a great deal"; No. 134, "I consider the operation entirely successful"; No. 140 (See Plate II, Figs. 1 and 2), "No question but that the operation, immediately, and apparently permanently, removes the trouble"; No. 141 (See Fig. 44), "Operation afforded me a very welcome relief after about four weeks of almost steady pain, and, although even now I do not put any more strain on my shoulder than I can help, it feels as strong as it ever did. I would not hesitate to undergo a like operation again to relieve like pain"; No. 142, "The result was most satisfactory. On only three or four occasions have I realized I had a shoulder and then only a slight soreness for a day or two after having used it perhaps a little too strenuously"; No. 143, "Good."
I am quite certain that most of my other patients to whom this questionnaire was not sent, or who did not reply to it, had as favorable results, because I have heard from most of them occasionally for many years after my operations. Details of some of these cases may be found in the Table on pp. 255-260.
I also have notes on about an equal number of cases who were not operated upon, usually because I thought the symptoms too trivial, but in some cases, because the patient refused operative treatment after having my assurance that in time they would recover at any rate. In most of these cases, especially in those in whom perforation had already occurred, the results have been as good as in those operated upon, although it seemed to me the patients suffered more. Many have recovered as promptly under some form of palliative treatment, as if I had operated upon them, but a few have had prolonged convalescences and suffered a great deal. My brother, a business man, had acute attacks in both shoulders for several months each, at different times. He would not sacrifice the time to be operated upon, but obtained some relief from diathermy. On the whole it seemed to me he suffered more than any case has suffered after the operation, but he did not lose a day. This was a subacute case with no restriction. As a rule I have operated on only the worst cases. In fact, I seldom advise operation unless the pain is severe. The unoperated series is, therefore, in the main composed of much milder cases, for those with severe pain welcomed operation.
For the sake of my argument that operation is wise in those cases where the pain is hard to bear, it is not necessary to attempt to contrast the periods of disability in an unoperated series with those that were operated upon, because the operated series shows many cases where the symptoms prior to the operation had existed much longer than they persisted in any case after it.
It does not seem to me worth while at the present time to go into this question in greater detail, because it is evident to me from a study of the unoperated cases that these patients eventually recover under any form of treatment which is not actually detrimental. The question is wholly one of relief of symptoms, not of the removal of a condition which is in itself dangerous or likely to lead to permanent disability. Although I am inclined to think that those cases which are not operated upon may ultimately have weaker tendons than those in whom the deposit is removed, I have no statistical proof of this, nor have I ever known of complete rupture of the supraspinatus occurring as an aftermath of this lesion. My reason for thinking that the tendons are weakened is more on account of the frequency of finding, at autopsy, defects which might be accounted for on this hypothesis.
Deposits in the Subscapularis. It may be that deposits in the subscapulars are less responsive to surgery than when they occur in the other tendons. I have had experience with only two cases, but they were both instructive to me, for I criticize myself for being content with removing one large deposit and making no effort to be sure there was no deposit in the other tendons.
Case No. 84. This was an acute case of two weeks' duration in a single woman of 46. I operated February 2nd, 1926, and removed a deposit from the supraspinatus. The result was satisfactory. However, about two years later, very acute symptoms returned in the same shoulder. This time the X-ray clearly showed a large deposit in the subscapulars and the remains of a smaller one in the supraspinatus. (Plate II, Fig. 6.) I operated again and removed the subscapularis deposit. The immediate result was as good as before, but the convalescence was more protracted in the subacute stage. She was an accountant and used the typewriter a good deal. She states that she went back to work two weeks after the first operation and four weeks after the second one, but her reply indicates some residual trouble: "Always occasional twinges since. Always 'cranky' as to normal use—have to turn certain way to put arm over and upward."
I am inclined to think that I might have saved this patient the second operation by a more careful X-ray study at the time of the first operation, for evidence of the other deposit may have been present at that time.
Case No. 117. A maiden lady of 64, who had a large calcified deposit in the subscapularis. (See Fig. 43.) She had had subacute symptoms for four weeks before the operation. According to her reply she had a longer and more stormy convalescence than any of my other cases have had; i.e., the acute pain after the operation lasted six days; the subacute pain three and a half months, and the occasional twinges ten months. It was a year before she forgot about the arm entirely. There have been no after effects.
This patient did not answer the question about the general impression of the efficacy of the operation, but it is clear that she suffered somewhat more after the operation than she did before it. She was operated upon in another city, and I did not have direct care of her convalescence, as I have in almost all the other cases. I was, however, in telephone communication with her doctor, and saw her from time to time during the year following. There seemed to be no very distinct reason why she should have had a longer convalescence than the other cases, but there were several possible reasons, which it seems worth while to discuss because they may have some future importance. In the first place, the deposit was in the subscapularis, a rather unusual situation. The operation was not difficult, because outward rotation of the arm easily brought the deposit under the wound which was made in the usual situation in the deltoid. I did not, in her case, incise any of the other tendons, and there may have been a tendinitis in those tendons which was the cause of the delay. Also, she did have some haematoma in the wound, which might have accounted for the postoperative pain being longer than usual. It is my usual custom to lightly bandage the arm to the side for the first night, and next morning to remove the bandage and allow the patient to place the arm in any position he chooses. There was some delay in removing the bandage in this case, I am told, because the patient seemed to have so much pain. It is possible, also, that the patient was one who, in her anxiety to be conscientious in her statements, has given an impression in the answer that her pain was greater than it was.
As these two cases were the only unsatisfactory ones I have had, and as they were the only ones in which there were large deposits in the subscapularis, it would be logical to attribute the slow convalescences to the location of the deposit. Two cases do not give much opportunity for logic when complicated by the factors of the personalities of doctors and patients. It may be that I could have saved both patients a considerable amount of pain by more thoroughness, and it may be that the two ladies were not of a satisfactory type for surgery, and would have been better satisfied with diathermy. At any rate, they represent my two worst results from operations for calcified deposits. In spite of the somewhat stormy convalescences I believe both patients were saved much suffering, for they seemed to me to be cases of severe type. The operation is a trivial one from a surgical standpoint, but to some people an operation is an operation, and those who would be inclined to take a surgical experience too seriously may well be treated with palliative measures.
BIBLIOGRAPHY FOR CHAPTER VI
ALLEN, A. R., Penn. M. J., 1911, xiv, 843; Therap. Gaz., 1911, 3, s., xxvii, 546. BAER, W. S., Johns Hopkins Hosp. Bull., 1907, xviii, 282-284. BERGEMANN and STIEDA, A., MUnchen med. Woch., 1908, lv, 2699-2702. BERRY, J. McW., Am. J. Orthop. Surg., 1916, xiv, 476-483. BETAGH, G-, Policlin., Roma, 1904, xi, sez, chir., 1930. BLANCHARD, W., J. Orthop. Surg., 1920, ii, 466. BOCK-OVEN, S., U. S. Vet. Bur. M. Bull., 1930, vi, 549-550. - BOU PUJOL, A., Arch, de ginecop., Barcelona, 1909, xxii, 99-104. BRENCKMANN, E., and NADAUD, P., Arch, d'elec. med., 1932, xl, 27-29. BRICKNER, W. M., Intern, clin., 1911, 1929; Am. J. Surg., 1912, xxvi, 196-204; Med. Rec, 1915, lxxxvii, 121 and 498; Am. J. M. Sc, 1916, cxlix, 351-864; Interstate M. J., 1915, xxii, 331-343; J. A. M. A., 1916, lxvi, 912; Am. Atlas Stereoroentgenol., 1916, i, 34-36; Am. J. Surg., 1916, xxx, 108-110; Am. J. Orthop. Surg., 1916, xiv, 231; J. A. M. A., 1917, lxix, 1237-1248; Midland M. J., 1918, xvii, 33-37. BROWN, A. J., Surg. Gyn. and Obs., 1919, xxix, 381-386. BUCHOLZ, C. H., J. A. M. A., 1917, lxix, 968; book, Lea and Febiger, 1917, Arch. f. klin. Chir., Berlin, 1922, cxxi, 255-264. BUCKLEY, C. W., Pract., 1914, xcii, 777-787; Proc. Roy. Soc. Med., London, 1913-14, vii, 59-70. BUTLER, P. F., and ELWARD, J. F., Am. J. Roent., 1925, xiii, 536-541. CALATUYAD, C, and ESTOPINA, L., Rev. espanol, de electrol y radiol. med., Valencia, 1912, i, 325-383. CAMPBELL, W. F., Med. Times, 1916, xliv, 244. CARNETT, J. B., and CASE, E. A., S. Clin. N. Am., 1929, ix, 1107-1126. CARNETT, J. B., S. Gyn. and Obs., 1925, 404-121; S. Clin. N. Am., 1930, x, 1309-1817; Radiology, 1931, xvii, SOS-SIS. CODMAN, E. A., Boston Med. and Surg. Jour., cl, 14, 371-374, 1904; Boston Med. and Surg. Jour., cliv, 22, 613-620, 1906; Records of the Massachusetts Medical Society, June 9, 1908; Boston Med. and Surg. Jour., Oct. 22, 29; Nov. 6, 12, 19, 26; Dec. 8, 1908. COLE, W. H., Surg. Clin. N. Am., 1923, iii, 1361-1363. COLLEY, F., Dtsch. Z. f. Chir., 1899, liii, 563-574. COMBEAU, Gaz. d. hdp., Paris, 1868, xli, 207. CONLOMB, Rev. d'orth., Paris, 1922, 3, s., ix, 251-253. COOPER-MAN, M. B., N. Y. State J. M., 1926, xxvi, 807-814. COUES, W. P., Boston M. and S. J., 1921, clxxxiv, 176-179. CUMSTON, C. G., Ann. Surg., 1913, lvii, 143. DAWBARN, R. H. M., Boston M. and S. J., 1906, cliv, 691. DAY, H. F., Boston M. and S. J., 1918, clxxviii, 389-392. DEERING, G. E., Phys. Therap., 1930, xlviii, 362-366; Am. J. Electrotherap. and Radiol., 1917, xxxv, 170-176. DESPLATS, H., J. d. sc. med. de Little, 1891, i, 265-271; Bull. off. Soc. franc, d'electro-ther., Paris, 1904, xi, 289-301; Ann. d'electrobiol., Paris, 1904, vii, 674-685. DIALTI, G., Cesalpino, Arezzo, 1908, iv, 169-176. DICKSON, J. A., S. Clin. N. Am., 1924, iv, 1053-1063. DOLLINGER, G., Orvosi hetil., 1932, lxxvi, 27-29; Zentrbl. f. Chir., 1982, lix, 579-583. DONLEY, J. E., Boston M. and S. J., 1911, clxv, 273. DOUGLAS, J., Ann. Surg., 1917, lxvi, 230. DUNLOP, J., Am. J. Orth. Surg., 1916, xiv, 102. DUPLAY, Rev. part. d. trav. de med., Paris, 1896, liii, 226; Semaine med., Paris, 1896, xvi, 193-194; Med. Week, Paris, 1896, iv, 258; Med. Press & Circ, London, 1900, n.s., lxix, 571-573. ECCLES, McA., West London Med. J., London, 1920, xxv, 87. ELMSLIE, R. C, Br. J. of Surg., 1932, xx, 78, 190-196. ELY, L. W., Am. J. Orth. Surg., 1914-15, xii, 447-450. ERB, K. H., and FRIEDRISZIK, W., Dtsch. med. Woch., 1982, lviii, 1004-1005. FALTA, Wien, med. Woch., 1920, lxx, 1414-1416. FIELDS, S. O., N. Y. M. J., 1915, ci, 163. FISHER, C. F., West Virginia M. J., 1927, xxiii, 250-252. FLINT, J. M., J. A. M. A., 1913, lx, 1224. FORT, F. T., Kentucky M. J., 1911, ix, 897-899; Railway Surg. J., 1912-13, xix, 8-14. FOWLER, E. B., Illinois M. J., 1932, lxi, 332-334. FRAUENTHAL, H. W., Internat. Clin., 1918, 28 s., iv, 60. FREUND, L., Wien klin. Woch., 1917, xxx,
665; Munch, med. Woch., 1917, lxiv, 784; Med. klin., Berlin, 1909, v, 387-390. FRIEDRISZIK, W., Rbnt. Med. Woch., 1982, Iviii, 1004. GALLOWAY, H. P. H., Canadian J. M. and S., Toronto, 1909, xxvi, 277-284. GARIBDJANJAN, G. A., Z. f. Orth. Chir., 1932, lviii, 48-53. GERSTER, A. G., Med. News, 1884, xliv, 428.
GIBNEY, H., Am. J. Orth. Surg., 1906-7, iv, 91-93. GIBSON, A., Canadian M. A. J., Toronto, 1928, xviii, 80-34; J. Bone and Joint Surg., 1922, iv, 552-559. GIBSON, H., Am. J. Orth. Surg., 1906-7, iv, 91-93. GILCREEST, E. L., S. Surg. Transact., 1981, xliv, 522-545. GONTIER, A., Union med., Paris, 1869, vii, 6-8.
GRACE, J. J., British M. J., London, 1914, i, 1012. GRANGER, L. B., Internat. Clin., 1926, 36, s., iv, 265-268. GROSSMAN, J., M. Times, 1928, lvi, 131-134. GUIBE, M., Rev. gen. de clin. et de therap., Paris, 1919, xxxiii, 408. GUNZ-BURG, J., Geneesk. Tijdschr. v. Belgie, Amsterdam, 1910, i, 36-39. HAENISCH, G. F., Fortschr. a.d. Geb. d. Roentg., Hamburg, 1910, xv, 293-300. HAMMER, A. W., Am. J. Surg., 1921, xxxv, 29-31. HAMMOND, R., Rhode Island M. J., 1917, i, 223. HARBIN, M., Arch. Surg., 1929, xviii, 1491-1512. HARRIS, J. F., J. A. M. A., 1923, lxxxi, 98; J. A. M. A., 1925, lxxxv, 1134. HARSHA, W. M., Internat.
Clin., 1919, 29, s., ii, 66-69. HAUSSLING, F. R., S. Clin. N. Am., 1926, vi, 1508-1528. HAYDEN, J. G., Railway Surg. J., 1917-18, xxiv, 8-11. VON HEDRY, N., Beitr. z. klin. Chir., Tubing., 1924, cxxxii, 244-247. HELLFORS, A., Med. Klin., 1930, xxvi, 309-311. HIRTZ, Soc. de med. mil. franc. BuU., Paris, 1912, vi, 277-
284. HITZROT, J. M., Min. Med. Cornell U. Med. Bull., 1928. HOGLER, F., Ars. med., Vienna, 1931, ix, 547-552; Arch. Innere Med., Vienna, obstr. J. A. M. A., 1928. HODGES, F. M., Virginia M. Month., 1925, lii, 155-156. HOLZKNECHT, G., Wien med. Wochr., 1911, lxi, 2757-2760. HOWARD, A. G., and HARVEY, C. D., Hahneman Month., 1915, 1, 323-833. HANCREDE, C. B., Internat. Encycl.Surg., 1895, vii, 395-402; 1882, ii, 691-733; 1884, iii, 105-147. ISRAEL, J. G., Internat. J. Surg., 1921, xxxiv, 8-14. JARJAVAY, J. F., Gaz. hebd. de med. et de chir., Paris, 1867, iv, 325-327, 357-359, 387-391. JONES, H. W., and ALLISON, N.,
N. Y. M. J., 1904, Ixxx, 930-934. JUNG, A., and BRUNSCHWIG, A., Rev. de chir., Paris, 1931, 1, 611-616. KAMMERER, F., Ann. Surg., 1917, lxvi, 112-115. KIENBOCK, R., Arch. f. phys. med. u. med. Tech., Leipzig, 1910, v, 98-99. KLEINBERG, S., Med. Rec, 1915, lxxxvii, 870-873. KOVACS, R., Phys. Therap., 1926, xliv, 90-109; 1927, xxxxvi, 181. KUSTER, E., Verhandl. d. dtsch. Gesell. f. Chir., Berl., 1902, xxxi, 364-372; Archiv. f. Klin. Chir., 1902, lxvii, 1018. KREUTER, E., Dtsch. Z. f. Chir., Leipzig, 1904, lxxii, 136-152. LAMY, L., and P^RES, P., Presse med., Paris, 1926, xxxiv, 739-740. LAVRAND, H., J. d. sc. med. de Lille,
1896, ii, 25-34. LEMONIE, Presse med. beige., Brux., 1904, Ivi, 660. LEONARD, T. B., Virginia M. Semi-Month., 1916, xxi, 349-350. LERICHE, R., and BRENCK-MANN, E., Lyon chir., 1931, xxviii, 281-285. LERICHE, R., and POLICARD, A., Masson et Cie., Paris, 1930, 69. VON LIEBERMANN, A., Med. Klin., 1930, xxvi, 1073; Munch, med. Woch., 1928, lxxv, 605. LITTIG, L. W., J. Iowa State M. Soc, 1913-14, iii, 625-630; Tr. West. Surg. Ass., 1913, 1914, 107-113, 117-124. LOTSY, G. O., Fortschr. a. d. Geb. d. Roentgenstrahlen, 1910, xvi, 158. LOVETT, R. W., Surg., Gyn. and Obst., 1922, xxxiv, 437-444. LOZANO, R., Clin, med., Zaragoza, 1914, xiii, 487-440. McGAULEY, F. F., N. Y. State Med. J., 1925, xxv, 472-474. MAGNUS0N, P. B., and COULTER, J. S., Intemat. Clin., 1920, iv, 203. MAIR, R., Ztschr. f. d. Ges. Avat., 1927, vxxxiv, 203. MARSHALL, H. W., Med. Rec, 1914, lxxxv, 280-289. MARTIN, P. F., J. Indiana M. Ass., 1910, iii, 109-117. MAUCLAIRE, Ann. de med. leg., 1932, xii, 471-472. MIGLIEWITCH, Arch, gen. de Kinestherapie, Paris, 1909, xi, 224-228. MONTGOMERY, A. H., J. Am. M. Ass., 1916, lxvi, 264. MOREN, J. J., Kentucky M. J., 1911-12, ix, 881-884; Louisville Month. J. M. and S., 1914-15, xxi, 68-75. MORRIS, J. M., M. J. Australia, 1926, i, 432-437. MOSCHCOWITZ, E., Am. Jour. Med. Sc., 1915, xv, 1-7. MU'LLER, A., Zentralbl. f. Chir., 1932, lix, 1810. MUMFORD, E. B., and MARTIN, F. J., J. A. M. A., 1931, xcvii, 690-694. MURPHY, J. B., Surg. Clin., 1915, iv, 661. NANCREDE, C. B., Internat. Encycl. Surg., 1882, ii, 691-733; Transl. Encycl. Internat. de chir., Paris, 1884, iii, 105-147; Internat. Encycl. Surg., 1895, vii, 395-402. NICHOLIS, S., Radiol, med. Milano, 1924, xi, 638-640. O'FERRALL, J. T., M. and S. J., 1925, lxxviii, 259-267. O'REILLY, A., and EWERHARDT, F. H., J. Missouri M. A., 1919, xvi, 149. ORR, T. G., J. A. M. A., 1923, lxxx, 1434-1436. PAAL, E., Arch. f. Orth. und Unfall Chir., 1932, xxxii, 100-106. PACKARD, G. B., Colorado Med., 1908, v, 5-9. PANNER, H. J., Hosp., Tid., Kobenh., 1912, v, R., v, 561-567. PAINTER, C. F., Boston Med. and Surg. J., 1907, clvi, 345-849. PAUS, M. Forh. med. Selsk. i. Kristiania, 1914, 135-138. PLUMMER, W. W., N. Y. State J. M., 1916, xvi, 203-208. POHL, R., Wiener Klin. Woch., 1930, xliii,
397-398. POPE, S. T., California State J. M., 1917, xv, 268. PUTNAM, J. J., Boston M. and S. J., 1882, cvii, 509, 536. RABINERSON, A. B., Vestnik khir., 1929, xvi, 100-103. RAMIREZ, Y. S., New Orleans M. and J., 1927, Ixxx, 324. RESNIK, J., Physical Therap., 1929, xlvii, 322-329. RICHARDS, T. K., New England J. of Med., 1931, ccv, 812-813. RUGH, J. T., Penn. M. J., 1911, xiv, 845-850. SADOLIN, F., Hosp. Ted., Kobenh., 1902, 4, R., x, 225-231. SCHLESINGER, A., Berlin Klin.Woch., 1908, xvi, 249-252. SCHREIBER, A., and HOFMEISTER, F., Syst. Pract.Surg., 1904, iii, 17-160. SCHWARZ, A., Wien, med. Woch., 1913, Ixiii, 1858-1857.SCHWARZ, E., Dtsch. Z. f. Chir., 1931, ccxxxv, 1-3; Dtsch. Z. f. Chir., 1932, ccxxxv, 140-163. SCHWYZER, A., St. Paul M. J., 1908, v, 45-48. SEGOND, Rev. gen. de clin. et de therap., Paris, 1910, xxiv, 785. SIEBERT, K., Fortschr. d.Med., Berlin, 1926, xliv, 509-515. SIEVERS, R., Dtsch. Z. f. Chir., Leipzig, 1914, cxxix, 583-653; Verhandl d. dtsch. Gesell. f. Chir., Berlin, 1914, xliii, 243-253. SIMON, S., Ztschr. f. d. Ges. Anat., 1926, lxxxi, 389. SKILLERN, P. G., JR., Internat. Clin., 1914, 24, s., ii, 233; Internat. Clin., 1913, 23, s., iii, 205. SMITH, M. K., Med. Rec, 1917, xci, 406-408. SMYTH, W. J., Practitioner, London, 1917,
xcviii, 575-576. STEINDLER, A., J. Orth. Surg., 1921, iii, 652. STERN, W. G., Surg. Gyne. and Obst., 1925, xl, 92-94. STEWART, J. E., South. M. J., 1928, xxi, 280-283. STULZ, E., and BRENCKMANN, E., Rev. d'orth., 1929, xvi, 481-489. SWETT, P. P., Yale M. J., 1910-11, xvii, 154-167. SZUBINSKI, A., Zentralbl. f. Chir., 1932, lix, 1638-1644. TAKAHAYASHI, K. A., Geibi Iji, Tokyo, 1900, xlix, 4-6. TAVERNIER, L., Bull, et mem. Soc. nat. de chir., 1932, lviii, 956-960. THOMAS, T. T., Am. J. M. Sc., 1911, xcli, 515-534; Therap. Gaz., 1912, 3, s., xxviii, 88-95; Therap. Gaz., 1913, 3, s., xxix, 229-247; J. A. M. A., 1914, lxiii, 1018-1025. TITUS, N. E., Am. J. Siirg., 1929, vi, 318-321; Brit. J. Actino-therap., 1930, v, 36. TUSZEWSKI, F., 8°, Greifswald, 1878. USLAND, O.,Norsk. Mag. f. Laegevidensk., Kristiania, 1920, lxxxi, 980. VADON, H., 4°, Mont-pellier, 1880. VALENTIN, B., Ztschr. Orth. Chir., 1931, lv, 229-240. VAN ASSEN, J., Nederl. Tijdschr. v. Geneesk., Amst., 1912, ii, 1517-1519. WALDEN-STROEM, J. A., Dtsch. Klin., Berlin, 1874, xxvi, 172. WATKINS, J. T., J. Bone and Joint Surg., 1925, vii, 787-789. WEISSENBACH, J. R., and FRANCON, F.,
Bull, et mem. Soc. med. d. hop. de Paris, 1930, liv, 1733-1738. WEISSENBACH, R. J., and TRUCHOT, P., Bull, et mem. Soc. med. d. hop. de Paris, 1931, xlvii, 1790-1793. WILSON, P. D., J. A. M. A., 1931, xcvi, 438-439. WILCOX, A. E., Minn. Med., 1928, vi, 245-247. WOJCIECHOWSKA, H., Lausanne, 1907, Ixxii, 8°.
WOLF, H. F., A. J. Surg., 1923, xxxvii, 59-62; N. Y. M. J., 1916, civ, 217. WORMS, G., Soc. de med. mil. franc. Bull., Paris, 1912, vi, 202-209. WREDE, Arch. f. Klin. Chir., 1912, xcix, 259. YOUNG, J. K., Therap. Gaz., 1917, 3, s., xxxiii, 1-4; Ann. Surg., 1916, lxiv, 368-871. ZOLLINGER, F., Arch. f. Orth., Munchen and
Berlin, 1927, xxiv, 456-467.
Almost all of the above articles are brief reports of the first few cases of calcified deposit which were observed in each locality, and give illustrations of the X-ray findings. In my opinion the articles by Brickner, Carnett, Harbin and Stieda are the most instructive. The article by Kiister in 1902 did not mention calcified deposits, but I am quite sure that the cases which he observed were such cases. His excellent and brief article was, so far as I know, the first rational description of subacromial bursitis. It was called to my attention some years after I had written my first paper, but was in fact written before mine.
Duplay's first article appeared in the Archives General de Medecin, Nov., 1872, but it apparently was not at first appreciated. Another paper in 1896 received more notice and literal translations were at once printed in two English Journals (see ref. above). Most European authors credit to him the introduction of the term "Periarthritis of the Shoulder" (periarthrite scapulo-humerale, periarthritis humero-scapularis). The chief advances in our knowledge of the subject since Duplay's contribution have been due to the use of the X-ray (discovered in Dec, 1895), so that we have been able to study separately the cases in which there is a calcified deposit or in which a fracture of the tuberosity had taken place. Except for that of Dickson and Crosby, quoted on page 224,1 have found no important study of the type of cases to be considered in the next chapter in which little if any calcification is found.
The articles by Baer and Painter both appeared in 1907 and I think were the first articles in this country to recommend surgical removal of the deposits. Bergemann and Stieda recommended surgery in Germany in 1908. Most of the articles advise some form of physiotherapy. It has seemed unnecessary to me to print the titles of all these papers on account of the large amount of space that this would require. Doubtless most of these authors would today be able to give as detailed a study as I have given in this chapter, but many of the articles show a lack of knowledge of minor points which have probably become plain to most of them during the intervening years. For instance, none of the articles seem to give proper consideration to the fact that nature's method of cure is by evacuation of the calcified material into the bursa. Many of the authors seem to think that the origin of the particles is in the bursa, and hence use the term "calcified bursitis." A good many attribute the onset of the trouble to recent trauma.
Most striking is the length of the bibliography of this chapter as compared to that of the last one on complete rupture of the supra-spinatus, which, to my mind, is so much more important and disabling a lesion than that caused by calcified deposits. The reader should refer to the comparison of costs on the scheme on page 124. Even the brief bibliography that I have given at the end of that chapter is partly composed of articles which really do not refer to the subject, and are only related to it. In fact, my papers and that of Wilson are really the only ones devoted to the subject. It seems to me most important for the profession to learn to differentiate between these two common causes of shoulder disability. As a matter of fact it is essential on the patient's account that rupture of the supraspinatus tendon should be recognized and operated upon promptly, whereas, the treatment of calcified deposits is a matter of choice, although my personal opinion is in favor of prompt surgical removal of the deposit. There is so little difference between the results of surgery and the results of any form of palliative treatment that I do not feel in these cases, as I do in those of ruptured supraspinatus, that their treatment is essentially surgical.
My own articles have been extensively quoted (often incorrectly) in American and English literature. This has been one reason why I have taken so much pains in this chapter to enter into the minor details of this comparatively insignificant lesion, cases of which recover in due time by nature's own methods. This chapter may also be of some importance because I am able to report the results of many cases which were operated on a long time ago. However, I feel that in some of these patients, whether or not operated upon, the tendons have probably been weakened through destruction of the tendon fibers so that had they been subjected to unusual trauma they might have ruptured more easily than normal ones. As stated in the chapter on Pathology, there is some doubt as to whether the defects so frequently found by Dr. Akerson may not have been sometimes due to destruction of the tendon by these calcified deposits years before autopsy. In the cases which I have reported as operated on for complete rupture, there was no doubt in my mind from the pathology found that the lesion was purely traumatic, although I could not, of course, determine whether there may not have been a weakened tendon before the actual rupture. In no case did I get a definite history of a calcified deposit in years previous to the rupture. Autopsy specimens from cases known to have had these calcified deposits in earlier years, and in whom there had been no operation or history of later trouble, might clear up this point.


