Arthroscopic Rotator Cuff Repair Technique
Lennard Funk
1. Indications:
Within the active population, no matter the patients age, an active sporting individual with a traumatic rotator cuff tear is an indication for arthroscopic rotator cuff repair. The reason for this is both pain and the functional demand of the patient. A sporting individual would require optimum strength of all their shoulder muscles for sports and overhead activities. Thus, a fully functional cuff is a necessity. Secondly, it has been proven that rotator cuff tears increase in size over time. Partial thickness tears progress to full thickness tears, and small full thickness tears progress to large to massive full thickness tears.
2. Arthroscopic Rotator Cuff Repair
The advantages of arthroscopic repair over open repair are:
- reduced morbidities, such as infection and wound complications.
- Ability to perform better soft tissue release of the cuff
- Treat associated pathologies, such as Labral and biceps lesions.
The results of arthroscopic repair have been shown to be as good as open repairs for the correct indications. Therefore, there is a low tolerance to offer surgical fixation by the arthroscopic Surgeon than the open Surgeon, with reduced morbidity and also earlier return to sporting activities. Therefore, this makes it a more popular approach than open surgery for sports and active people.
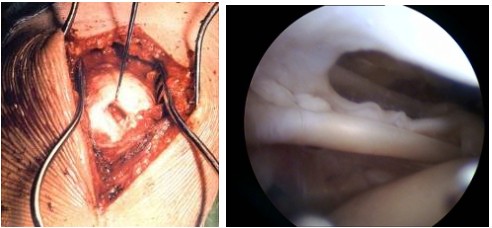
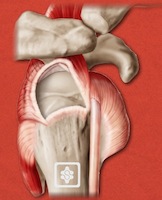
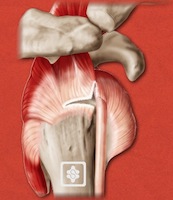
Rotator cuff tear open surgery on the left and arthroscopic view on the right
3. Pre-operative Investigations:
Clinical signs are useful for determining rotator cuff pathology but ultrasound scan or MR scan is unable to clearly delineate tear size, configuration and associated conditions. Ultrasound scanning has the advantage of being quick and safe, often performed by the Clinician themselves. The tear size can be determined and biceps pathology can also be identified. Muscle changes cannot be seen on ultrasound scanning at present.
MR scans are more costly, slower and can be associated with claustrophobia. However, they do show the muscle changes, such as muscle atrophy and fatty degeneration, which are helpful in prognosticating the results of rotator cuff repair.

Office Ultrasound scanning can be performed by the trained surgeon
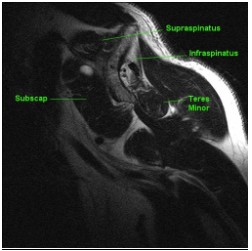
Muscle atrophy of Supraspinatus on MR scan
4. Beach Chair Position:
The 2 common positions for shoulder arthroscopy are the beach chair position and lateral position. My preference is the beach chair position, which offers the advantage of being more anatomical. It allows for a single position for all surgery. Therefore, one is able to undertake all open procedures, arthroscopic procedures or combined surgery at the same time. It is simple for the Anaesthetic staff and Nursing staff. I prefer to use light traction, simply holding the arm in a neutral position and freeing yourself of an assistant. It also has the advantage of being able to move the arm in rotation, abduction and adduction to obtain a better view. When it is often required to change portals regularly when performing an arthroscopic cuff repair, this can easily be done in the beach chair position.

5. Portals:
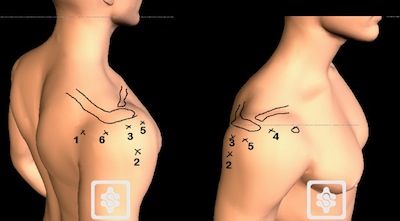
5.1. Posterior Portal:
My preferred starting portal is the standard posterior portal, 2 finger breadths below the posterolateral corner of the acromium and 2 finger breadths medial to this line (in the soft spot). This gives the ability for a initial glenohumeral arthroscopy for the diagnosis of possible associated glenohumeral articular cartilage damage, labral tears and the opportunity to assess the rotator cuff tear from its under surface, along with the intra-articular longhead of biceps tendon and subscapularis.
5.2. Lateral portal:
The 2nd portal utilised is the standard lateral portal, which is 2 finger breadths posterior to the anterior lateral corner of the acromium and 4 finger breadths inferior to the lateral border of the acromium. This portal can be utilised for:
1: Initial traction and debridement of the rotator cuff tendon edges.
2: Preparation of the bare area.
3: Release of adhesions and bursectomy.
4: Positioning with the scope for a 50 yard direct lateral view.
5.3. Superior lateral portal:
This portal is made 2 finger breadths posterior to the anterolateral corner of the acromium and 2 finger breadths lateral to the lateral border of the acromium. This portal is utilised for anchor insertion and knot tying, obtaining a good 45 degree dead-mans angle for anchor insertion.
5.4. Anterior portal:
This portal is made 2 finger breadths anterior to the acromioclavicular joint. This portal is utilised for instrumentation from anteriorly suture passing through the anterior rotator cuff edges and biceps tenodesis.
5.5. & 6. Anterior and posterior accessory the lateral portals.
These portals are made 2 finger breadths lateral to the anterolateral corner of the acromium and posterolateral corner of the acromium. These portals can be used for additional anchor insertion, along with additional instrument passing and knot tying as necessary. For a <2cm size rotator cuff tear, usually only the first 4 portals are utilised. For a larger cuff tear, including biceps tenodesis and or subscapularis tendon repair, all 6 portals are used. Additional accessory portals useful are the Nevasier portal and accessory posterolateral portal.
6. Surgical Procedure
6.1 Glenohumeral Arthroscopy
The glenohumeral joint (GHJ) is first inspected via the posterior portal. The undersurface of the rotator cuff can be inspected and the tear appreciated from the joint side. One is able to see the relationship of the tear to the long head of biceps tendon (LHB). The Subscapularis tendon can be examined and repaired from within the GHJ. The labrum and articular surfaces can be assessed. Labral tears and articular cartilage lesions can be treated before proceeding to the cuff repair.
From within the GHJ, the supero-lateral can be created from outside-in. Via this portal the following can be done:
a. The tear can be assessed for mobility using a grasper
b. The tendon edges can be debrided
c. The tear can be mobilised, releasing adhesions to the capsule and labrum
d. The footprint area of the tuberosity can be prepared for the repair
e. The LHB can be tenodesed or tenotomised, if required
6.2 Bursoscopy & Anterior Releases
The bursa is then entered via the posterior portal and the superior surface of the cuff assessed.
The true lateral portal is created. Via the lateral portal:
a. Anterior bursal adhesions can be removed, as necessary, using a soft tissue shaver and/or radiofrequency device:
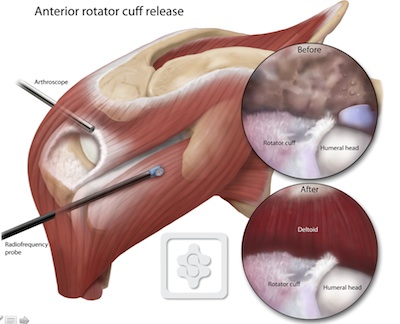
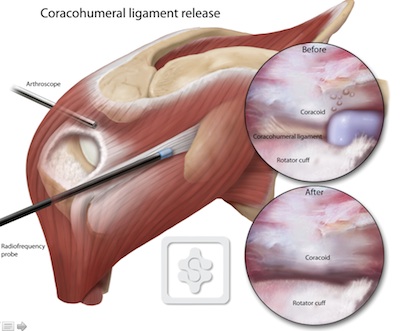
b. The coracohumeral ligament is released:
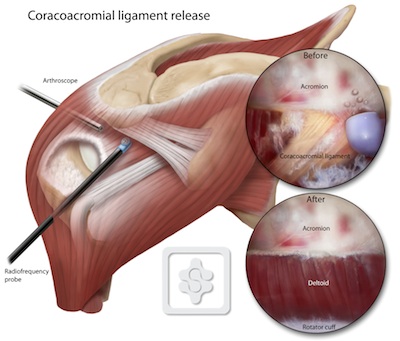
c. The coracoacromial ligament is released:
For a small (<2cm) tear I would now insert an anchor (5mm screw-in type) from the supero-lateral portal.
6.3 Release & Preparation viewing from Lateral
The viewing scope is then transferred to the lateral portal, giving the 50 yard view of the front and back of the tear, as well as the footprint area.
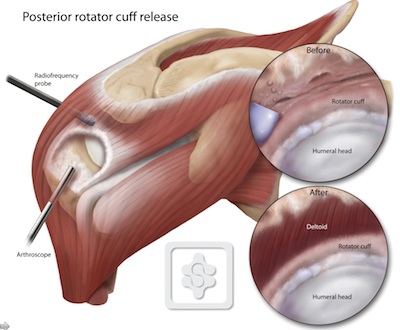
Posterior bursal adhesions are now released via the posterior portal, freeing the posterior cuff:
The anterior portal is now created for instrumentation and suture passing.
For small tears, a suture passer can now be passed from the anterior and posterior portals, retrieving sutures from the anchor. Simple suture repair, mattress repair or a modified Mason-Allen (locking) repair can be performed.
Careful suture management is essential here and some of the key points are:
a. Never have more than 2 suture limbs in a single portal
b. Ensure sutures are not twisted or caught in soft tissue before tying
c. Tie knots via the supero-lateral portal
6.5 Repair Techniques
The repair technique will depend on the tear pattern and reducibility of the tendon once it has been mobilised.
The standard cuff tear patterns are:
- Small crescent (U) tear
- Moderate crescent tear
- Large U-shaped tear
- V-shaped tear
- L-shaped tear
- Reverse L-shaped tear
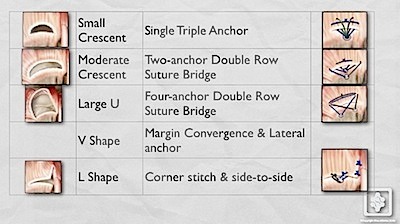
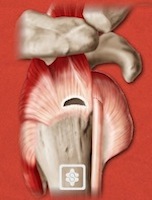
6.5.1. Small crescent tear = single triple-loaded anchor in a modified Mason-Allen pattern:
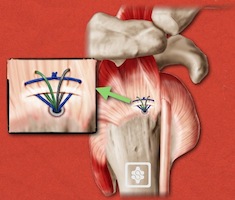
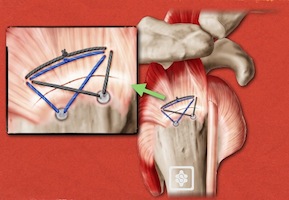
6.5.2 Moderate crescent (U) tear = Two anchor double row suture bridge technique:
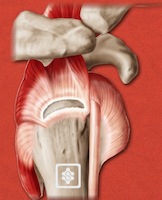
6.5.3 Large U tear = 4 anchor double row suture bridge technique:
![]() CLICK FOR VIDEO
CLICK FOR VIDEO
![]() CLICK FOR ANIMATION
CLICK FOR ANIMATION
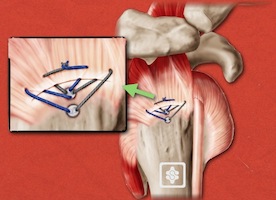
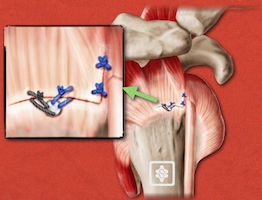
6.5.4 L-shaped tear = Margin convergence and lateral anchor:
![]() CLICK FOR VIDEO
CLICK FOR VIDEO
7. Post-Operative Rehabilitation
I use an customised, patient-specific rehabilitation program for arthroscopic rotator cuff repairs , as the fixation is strong and the deltoid is not disturbed. It is not 'accelerated' or 'aggressive'. Closed chain exercises in a safe range of motion can commence early after surgery to avoid stiffness and place light strain on the repair to enhance healing. Passive stretching and resistance must be avoided for at least 6 weeks after surgery. This is based on the EMG studies of Prof. Tim Uhl in the USA. Patients may begin full passive and active-assisted motion exercises immediately post-op, as tolerated. Isometrics are added before 3 weeks. They progress to active motion after 3 weeks and resistance exercises after 6 weeks. Athletes may return to overhead and contact sports after 3 months.
8. Orthobiologic Patch reinforcement/reconstruction
For some massive irreperable rotator cuff tears in young, active people with good quality cuff tissue reconstruction with a collagen patch is used. The aims of this are to provide a biological scaffold for tissue regeneration and anatomically reconstitute the mechanics of the cuff. I prefer to do this arthroscopically to prevent damage to the important deltoid muscle and allow early rehabilitation. Below is our (simple) technique:


