Arthroscopic Rotator Cuff Repair Results
Arthroscopic repair of the rotator cuff: Analysis of outcomes and factors that predict prognosis. Audit over 18 month period.
Cheryl Godley & Lennard Funk, 2009
|
Abstract |
Abstract
Aims:
The aim of this study was to audit the results of arthroscopic rotator cuff repair by the senior surgeon (Lennard Funk) and to analyse the results to ascertain whether there are any significant predictors of outcome of repair, such as age, sex, tear size, preoperative tissue quality and tendon retraction.
Methods:
110 patients operated over a 20 month period by the senior surgeon were included in the study.
Outcome measures used were pre-operative, post-operative and current Oxford and Constant shoulder scores as well as patient satisfaction. A questionnaire was sent to patients whose contact details were available to determine current Oxford and Constant which also included questions about smoking status, arm dominance and post-operative satisfaction.
Statistical analysis was done with SPSS version 16.0 for Windows.
Results
The mean follow up period was 36.5 months. All the patients had a significant improvement in Oxford and Constant scores from pre-operatively to 3 months post-operatively and at final review. No variables were found to have a significant effect on post-operative Constant and Oxford scores although size of tear had a borderline significant effect on patient Constant Score outcome at 3 months compared to pre-operatively.
Patients showed mean >80% improvement in their shoulder since the operation, the majority said they felt 'much better' and most had returned to the 'same' occupation/activities of daily living as pre-operatively.
No association was seen between age, sex, smoking status, arm-side or dominance and, tendon retraction, concurrent biceps treatment and pre-operative tissue quality on outcome.
Conclusions
Results of arthroscopic rotator cuff repair have been shown to give our patients significant improvement in shoulder function at 3 months and ongoing.
Introduction
The aim of rotator cuff repair is to relieve pain, restore strength, function and range of movement. Surgery to repair the rotator cuff has reportedly been performed for almost 100 years with the first open repair done in 1911 (Yamaguchi et al 2003). In recent years total arthroscopic repair of the cuff has replaced open and mini open repair techniques although this procedure still includes the fundamental techniques originally described by Neer in 1972. These include the preservation or repair of the deltoid origin, adequate subacromial decompression with removal of any osteophytes, surgical release in order to attain freely mobile tendon-units, secure fixation of the tendon to the greater tuberosity and a strictly managed rehabilitation protocol (Yamaguchi, 2003). The senior surgeon's technique encompasses all of these principals when repairing the cuff as well as treating any associated pathologies such as labral or biceps lesions found at the time of surgery.
There are a number of advantages of arthroscopic repair compared with older techniques. Studies comparing the mini-open repair and complete arthroscopic repair have found that the mini repairs has had slightly higher rates of revision rotator cuff procedures, infection and frozen shoulder requiring further manipulation under anaesthesia (Nho et al 2009).
Other advantages seen with arthroscopic repair are that it requires smaller incisions than open techniques whilst still enabling a good view of the glenohumoral joint and allowing other intraarticular pathology to be dealt with, and also it does not require deltoid detachment (Gartsman et al 1998).
Deltoid detachment is a complication of open rotator cuff repair and often occurs if the deltoid is not properly reattached during initial surgery and can cause pain and activity restriction and may require further surgical repair. Gumina et al found that patients who had deltoid detachment postoperatively had significantly less improvement in Constant score than those who did not have this complication. Fortunately arthroscopic repair does not require any surgery to deltoid thus does not have this complication.
Postoperative rehabilitation of the rotator cuff is essential to ensure that the tear heals successfully and should involve physiotherapy with extensive strengthening exercises and often a sling. It is important that rehabilitation protocols are strictly followed and exercises done for at least a year to give maximal improvement to shoulder function. These exercises help to strengthen the shoulder and passive movements should be instituted early to prevent problems such as shoulder stiffness (Lee and Flatow, 2005). Initiating active movements of the shoulder too early, lifting weights and removing shoulder brace too early can disrupt healing and lead to failure of repair (Brems, 2003).
Past audits of the senior surgeon's results have showed his rotator cuff repairs to be to be successful.
This study aims to add to those studies by aiming to identify if individual patient variables have an effect on the result of surgery.
The initial hypothesis and senior authors opinion was that patients who had poor tendon quality pre-operatively will have poorer outcomes and higher rates of retear and/or unsatisfactory results at follow-up.
Methods
We audited the results of arthroscopic repair of the rotator cuff by the senior surgeon performed over an 18 month period between 2005 and 2007, assessing preoperative, intraoperative and postoperative patient factors. The preoperative factors included the individual variables that may affect the outcome of repair. These include age, sex, smoking status of the patient and I also analysed pre-operative Oxford and Constant Scores. Intraoperative factors were size of tear, dominant or non-dominant arm operated on, quality of the cuff tissue, number of tendons involved, co-existing pathology to long-head of biceps and tendon retraction. Postoperative factors were follow-up Oxford and Constant scores, percentage improvement, return to activities of daily living and patient satisfaction.
The outcome of this audit will be used to identify if there are specific factors that result in poorer outcomes of arthroscopic rotator cuff repair and this may allow us to implement a different management strategy for such patients in the future.
Patient Selection
The patients included in the study were all those who underwent arthroscopic repair of the rotator cuff by the senior surgeon during an 18 month period between 2005 and 2007. Patients all had rotator cuff pain and functional impairment. All had a traumatic rotator cuff injury. All of the patients included have had a minimum of 1 year follow-up.
All patients were advised to follow a strict postoperative rehabilitation protocol which was usually arranged between the senior surgeon and a physiotherapist. Patients had to wear a shoulder sling for a minimum of 3 weeks post-operatively. After the operation patients were advised not to drive for a minimum of 6 weeks and the senior surgeon generally advised the patients when it was suitable to return to work depending on their individual job. For example patients whose jobs involved heavy manual labour were advised not to return to work for at least 8 weeks. The surgeon also gave patients specific advice on when to return to individual sporting activities.
Clinical data
To determine the success rate of each procedure we evaluated the pre and post operative Oxford and Constant scores (OS and CS) and these were the primary outcome variables. These were performed at 3, 6 and 12 months postoperatively. Patients over 12 months from surgery were contacted for up to date outcome assessments.
Patients' who had contact details available were contacted over the phone and current Oxford and Constant scores as well as post operative satisfaction were established. Patients who did not have telephone numbers available were sent a questionnaire if a follow-up address was available. Those patients, who could not be contacted by telephone, either due to change of address or failure to contact them after 4 unsuccessful attempts, were also sent a questionnaire to their home address if it was available. I included a stamped addressed envelope along with my questionnaire to encourage patients to respond.
Both Oxford and Constant scores are validated methods of shoulder assessment in relation to rotator cuff pathology and the scoring systems were used to conclude if the results of repair were satisfactory or not. The Constant score first published in 1987(Constant C.R, Murley A.H) and is one of the most widely used methods of assessing outcome after shoulder surgery. The Oxford score is also used in many countries worldwide and assesses patients' subjective level of pain and the level of impairment to their activities of daily living. The questionnaire is made up of 12 questions, one third related to pain and the other 2/3rds to activities of daily living (ADL). The maximum Oxford score is 60 points which applies to the worst possible outcome.
The Constant score is a detailed assessment of shoulder function with both subjective and objective components. The subjective variables that analyse pain and ADL constitute 35 points, and the objective variables that analyse range of motion and strength constitute 65 points, therefore there is a total of 100 points with 100 being the best outcome. A constant score of 65 or more and an Oxford score of 33 or less gives a good/excellent operative outcome. Pre-op, 3month, 6 month, 1 yr and current Oxford and Constant scores were studied however when analysing the effect of any independent patient variable on Constant and Oxford Scores I used the 3 month shoulder scores as my outcome measure as this had the highest response rate.
Patient satisfaction was assessed post-operatively and at present. This was determined by asking patients' how their shoulder felt following the operation: much better, better, same or worse; the percentage improvement they experienced; and whether they had returned to the same, reduced, different or stopped completely their previous occupation/activities of daily living due to their shoulder.
In the follow-up assessments we also asked patients about current or past smoking status to ascertain whether this has an influence on the outcome of primary repair. It is a concern that cigarette smoking may have an effect on tendon healing thus lead to poorer repair outcome. The arm which was operated on and arm dominance was also asked in the questionnaire.
Statistics
Statistical analysis was performed using SPSS version 16.0 for Windows. Descriptive statistics included means and frequencies. Independent sample t-tests, one way ANOVA and Repeated measures ANOVA were used to investigate potential predictors of surgical outcome by looking at the difference in shoulder scores from pre-operatively. Results were considered to be statistically significant at p<0.05.
Results
There were 110 patients involved in our study and they underwent rotator cuff repair in a 20 month period between 2005 and 2007. The primary outcome variables we looked at were pre and postoperative shoulder scores.
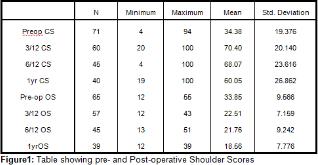
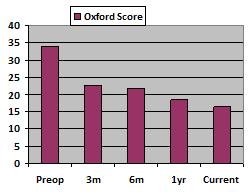
Figure 2: Graphs showing mean Constant and Oxford Scores 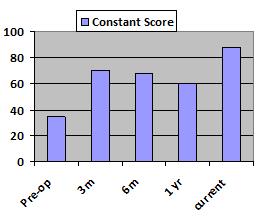
Of the 58 patients with 3 month Constant Scores 36 (62.1%) had Good/Excellent scores (>65). Of the 45 patients with 6 month CS recorded 31 patients (68.9%) had good or excellent scores.
Of the 57 patients with 3 month Oxford Scores recorded 54 patients (94.74%) had good/excellent scores (<33). At 6 months, of the 45 patients with OS recorded 40 (88.89%) had good/excellent score. At 1 yr 40 patients had OS recorded and of these 35 (87.5%) had good/excellent scores.
Repeated Measures ANOVA analysis comparing preoperative with 3 month Oxford and Constant score showed that there was a significant improvement found in both scores (p=0.0001) for both outcome measures. This shows that patients significantly improved from preoperatively to 3 months postoperatively.
Oxford and Constant Scores at 36.5 months:
| Minimum | Maximum | Mean (Std Dev) | |
| CS | 17 | 100 | 87.5 (18.5) |
| OS | 12 | 46 | 16.2 (7.7) |
The mean current Oxford and Constant scores both confer a mean good/excellent operative outcome.
Repeated measures ANOVA comparing pre-operative to follow-up Constant and Oxford scores showed significant difference in outcome for both outcome measures (p=0.0001). The mean follow up time of the patients who responded was 36.48 months (range 27 to 48 months) post-operatively and this significant result demonstrates that our patients have a tendency to keep improving over time.
Effect of age on shoulder scores
The average age of our patients at surgery was 56.7 years. 80 (72.7%) of the patients were under 65 years and 30 (27.3%) were over 65 years.
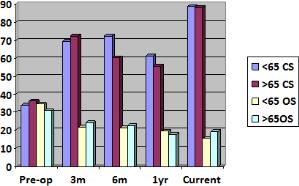
Independent sample t-test showed no statistically significant association between age on either Oxford or Constant Scores at 3months.
Gender
Gender is another variable I looked at to determine whether it had an influence on outcome of repair. Out of the 110 patients audited 29 (26.4%) were female and 81 patients (73.6%) were male.
When effect of sex on 3 month Constant and Oxford score was analysed by independent sample t-test no statistical significance found using the 95% confidence interval, showing that sex did not impact the outcome of surgery as measured at 3 months.
Operative Findings
The size of the tear for all 110 patients was assessed in theatre and recorded in the surgical notes.
Of the 110 patients 13 patients had massive tears (>5cm), 32 patients had large tears (3-5cm), 58 patients had moderate tears (1-3cm) and 7 patients had small tears (<1cm). This shows that the majority of the patients had moderate sized tears, (52.7%). While only 6.4% of the repairs were done to small tears which show that small tears can still cause functional problems and highlights the fact that size of anatomic defect does not always relate to the clinical picture.
Figure 6: Pie chart of size of tears in our patients 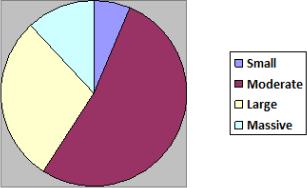
The following tables compare the mean Constant and Oxford Scores in patients pre-operatively, 3 months, 6 months and 1 year post-operatively and at final review to the tear size of the patient.
| OS | Small | Moderate | Large | Massive |
| Pre-op | 35 | 34.67 | 31.91 | 36.4 |
| 3m | 21.5 | 21.5 | 24.16 | 24.17 |
| 6m | 16.5 | 16.5 | 21.22 | 28 |
| 12m | 19 | 16.54 | 22.33 | 18.33 |
| 36.5m | 17 | 14.6 | 17.06 | 21.25 |
| C S | Small | Moderate | Large | Massive |
| Pre-op | 33.75 | 34.51 | 35.7 | 27.8 |
| 3m | 88.75 | 72.39 | 63.47 | 69.83 |
| 6m | 84 | 71.45 | 62.61 | 67.8 |
| 12m | 91 | 59.21 | 55.58 | 61 |
| 36.5m | 81 | 91.6 | 85.76 | 79 |
One way ANOVA analysis showed a borderline significant relationship between tear size and the difference in patient Constant score from pre-operative to 3 months (p=0.065) although this was not seen for the Oxford score. A Multiple linear regression analysis was performed to see if there was any further association between tear size and outcome and it also showed borderline significant result when comparing pre-operative to 3month Constant scores (p=0.057). This gives us some suggestion that tear size has an effect on patient outcome.
Is there a relationship between gender and size of tear ?
Comparatively similar numbers of male and female patients have suffered massive moderate and small tears showing that sex does not have an influence on the degree of rotator cuff injury and statistical analysis did not show a significant association between them. Interestingly more males suffered large tears but comparable numbers of males and females suffered massive, moderate and small tears.
Effect of pre-operative tissue quality on outcome of repair
The pre-operative quality of cuff tissue may play an important role in the outcome and success of the repair of the torn tendon and this was recorded in theatre. 1 (1.1%) of our patients had degenerative tissue, 21 (23.08%) had tissue that was poor and thinned, 35 (38.46%) patients had intermediate and delaminated tissue, 34 (37.36%) had good and thick tissue. Quality of cuff tissue was not recorded in 19 patients.
| C S | Good Thick | Int Delam. | Poor Thin | Degen. |
| Pre-op | 35.69 | 29.05 | 36.36 | 28 |
| 3m | 69.53 | 69.88 | 63.5 | 91 |
| 6m | 70.2 | 74.01 | 52.57 | |
| 12m | 63.79 | 54.94 | 59.5 | 85 |
| 36.5m | 90.2 | 89.4 | 87.75 | 94 |
| O S | Good Thick | Int Delam. | Poor Thin | Degen. |
| Pre-op | 33.8 | 35.79 | 32.45 | 45 |
| 3m | 22.73 | 23 | 22.7 | 20 |
| 6m | 21.1 | 19.82 | 25.91 | 14 |
| 12m | 19.46 | 18.18 | 22.25 | |
| 36.5m | 15 | 15.85 | 16.25 | 16 |
One-way ANOVA analysis did not show a significant association between tissue quality and outcome of repair.
Supraspinatus is generally the most commonly torn tendon of the rotator cuff. The location of the tear was recorded in 47 of our patients in theatre (42.73% of sample). 23 tears were to supraspinatus alone, 23 to both supraspinatus and infraspinatus and 1 to subscapularis. The site of tear was not analysed as a potential predictor of repair outcome but it is interesting to note that supraspinatus was involved in the majority that had location of tear recorded which we may expect.
Tear shape was recorded in 104 0f the 110 patients. 20 patients (19.2%) had 'L' shaped tears, 75 (72.1%) had 'Crescent-shaped' tears, 7 patients (6.7%) had 'inverted L-shaped' tears, 1 patient (0.96%) had a longitudinal split and 1 tear was described as 'combination'. Tear shape was not analysed but it is interesting to note that the majority of the patients had 'Crescent-shaped' tears.
Co-existent Biceps Pathology
Of the patients in our study 45 had treatment to biceps tendon. 34 had tendonesis, 4 had tenotomy and 7 had debridement of the tendon. Usually tendonesis is the treatment of choice in more active individuals as modern techniques give a strong repair that allows for early return to movement postoperatively.
One-way ANOVA analysis did not show a significant relationship between co-existing treatment of biceps tendon or need for biceps tendonesis and either outcome measure.
Retraction
The degree of retraction of the damaged tendon was recorded in all but 2 of the patients. 32 patients had damaged tendon but no retraction, 20 had stage I (mild) retraction, 22 had stage II (moderate), 18 had stage III (severe), 10 had stage IV massive retraction, 4 had retraction to less than 1cm and 1 had retraction of less than 5cm of subscapularis, and 1 patient had retraction that extended to the glenoid that was more than 5cm. To simplify statistical analysis degree of retraction was divided into 4 groups.
One-way ANOVA analysis showed no significant association between degree of tendon retraction and outcome at 3 months.
Smoking Status and Arm Undergoing Surgical Repair
No significant association was found between smoking status and postoperative outcome. Smoking status was recorded in 49 of the returned questionnaires. There were 29 (59.18%) non-smokers, 17 (34.69%) ex-smokers and 3 (6.12%) current smokers.
60 of the 110 patients (54.55%) had their right arm operated on and 50 patients (45.45%) had their left arm operated on. From the results of the questionnaire 23 patients had their dominant arm operated on (46%), 26 patients (52%) had their non-dominant arm operated on and 1 patient (2%) reported being ambidextrous.
There was no significant association found between the arm operated on and whether it was the dominant side on the postoperative outcome.
Patient Satisfaction and Return to Activities of Daily Living
Patient satisfaction in terms of percentage improvement since the operation, how their shoulder felt following the operation and return to activities of daily living were descriptive outcome measures used.
97 patients had percentage improvement recorded at their last follow-up post-operatively and the mean score was 80.21% (range 0-100). Percentage improvement was also asked in the questionnaire and the mean score calculated from the results of the 50 patients was 85.78%.
At final follow up and in the questionnaire patients were asked if they felt that their shoulder was much better, better, the same or worse since the operation. The majority of patients reported their shoulder as being 'much better' with very few reporting that it was 'worse' following the operation at both times of follow up.
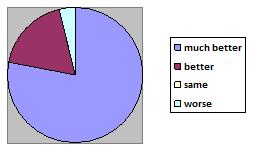
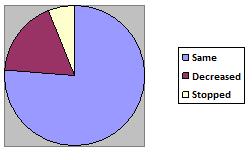
Patients were also asked about the effect their shoulder had on their activities of daily living at last follow up and in my questionnaire. The following pie charts show whether they had returned to same occupation/activities as before, a decreased level or stopped completely because of their shoulder:
These results show that on average patients were very satisfied with their shoulder postoperatively, that the majority had significant improvement in shoulder function and most had returned to their previous occupation or activities
Patients who required revision surgery
7 of the 110 patients (6.4%) required further revision surgery due to failure of repair or unsatisfactory results. 2 of these patients (28.57%) were female and 5 (71.43%) were male.
The patients who had to undergo revision rotator cuff repair were all over the age of 50 with the average age being 62.57 years. 5 (71.4%) of the 7 patients were under 65 years old therefore we can conclude again that age does not have a significant effect on surgical outcome.
The size of tear in these patients was as follows: 4 had large tears (57.14% of revisions and 12.5% of total with large tears), 2 had moderate tears (28.57% of revisions and 3.45% of total moderate tears), and 1 patient had a massive tear (14.29% of revisions and 7.69% of massive tears). No patients in the failed group had small tears. This is interesting as it suggests that there may be a link between tear size and outcome.
Of these patients 6 had tissue quality recorded. It was intermediate and delaminated in 3 patients (50%), poor and thinned in 2 patients (33.33%) and good & thick in 1 patient (16.67%).
5 of the 7 patients had treatment on biceps tendon: 4 patients required tendonesis and 1 had debridement of the tendon.
5 patients (71.43%) had tendon retraction and 2 had damaged tendons but no retraction. Of the patients with retraction 2 patients had stage IV (massive) retraction, 1patient had stage III (severe) retraction, 1patient had stage II (moderate) retraction and 1 patient had stage I mild retraction.
| Minimum | Maximum | Mean (Std Dev) | |
| CS Preop | 18 | 42 | 27.6 (8.85) |
| CS 3m | 20 | 98 | 62 (39.4) |
| CS 6m | 4 | 81 | 51.3 (41.43) |
| CS 12m | 19 | 51 | 35 (22.62) |
| OS Preop | 36 | 40 | 38.5 (1.73) |
| OS 3m | 15 | 30 | 23.67 (7.77) |
| OS 6m | 19 | 51 | 31.3 (17.21) |
| OS 12m | 29 | 34 | 31.5 (3.53) |
These figures emphasise that the patients who required revision surgery had much poorer Oxford and Shoulder score outcomes in comparison to the patients who had successful rotator cuff repair.
Discussion
Summary of Findings
This audit has shown that arthroscopic repair of the rotator cuff leads to significant improvement in shoulder function in terms of the Constant and Oxford shoulder scores. A significant improvement (p=0.0001) was seen from pre-operatively to 3 months post-operatively and patients' continued to improve over time which was seen when pre-operative results were compared to the shoulder scores calculated from the questionnaires in which patients had a mean follow-up time of 36.48 months.
In our group of patients there was no significant predictor of poorer outcome found when looking at both shoulder scores. Tear size was found to be a borderline significant predictor of outcome at 3 months and should be investigated further.
The mean percentage improvement our patients had since the surgery was very high at 80.21% and 85.78% at last follow-up and from current questionnaire respectively.
The majority of patients had returned to the same occupation/activities of daily living at last follow-up and currently from results of the questionnaire (69.56% and 76% respectively). 68.04% and 78% of patients reported there arm as being 'much better' following the operation at last follow-up and from questionnaire results, which again highlights the success of the surgery.
Review of the literature
Several factors have been implicated in the past as predisposing to failure of rotator cuff repair and/or a persistent defect post-operatively. The study by Nho et al 2009 showed that increased age and size of tear pre-operatively significantly increased the risk for a defect post-operatively.
Bishop et al (2006) compared both open and arthroscopic rotator cuff repair found that both methods were comparable and gave satisfactory clinical results. The study also showed that patients with tears less than 3cm had a 'higher rate of rotator cuff integrity' than those with larger tears and thus had a lower retear rate. Strength of forward elevation and external rotation was also found to be higher when the tear was less than 3cm and if the cuff remained intact after repair.
Study by Burkhart et al (2001) disagrees with this and concluded that the outcome of arthroscopic repair is completely independent of the size of tear.
My results showed a borderline significant association of tear size on the difference between 3 month and pre-operative Constant scores , p=0.065 when analysed by one-way ANOVA and p=0.057 when multiple linear regression analysis was performed, so one may conclude there is some suggestion that tear size has an effect on operative outcome. This finding was not significant when Oxford Score was analysed as the primary outcome measure. However overall, Oxford scores were superior in patients compared to Constant scores so a significant result is less likely for this outcome.
Our results showed that Oxford Score was highest pre-operatively in the group with massive tears as we may expect. It is interesting to note that the group with least improvement in OS was large tears. However for all sizes of tear the mean 3 month Oxford score was =33 thus construing a good/excellent operative outcome
The Constant scores of our patients improved from pre-operatively for all tear sizes and the 3 month Constant scores was =65 in all but the large tear size group. Interestingly the mean scores were good/ excellent in the massive tear group and were actually better than in patients who had large tears which we may not have expected from what has been reported in the literature. Although this result may be due to the small number of patients who had massive tears compared to those with large tears.
Out of the patients who required revision procedures none had small tears, 4 had large tears, 2 had massive tears and 1 patient had a moderate tear. It is interesting that no patients had small tears and I think that the potential association between tear size and outcome needs be further investigated.
Razmjou et al (2009) performed a study that looked specifically at the relationship between patient sex and the outcome of repair and found that females reported higher levels of disability and restriction to activities than males despite having similar or lower levels of pathology.
Our results refute the finding that sex has an affect on the outcome of repair and a relationship was not seen between the two. Interestingly I also found that the number of males and females required revision surgery (28.57 and 71.43% respectively) was comparative to the total number of females and males who initially underwent arthroscopic repair (26.4% and 73.6% respectively). This further emphasises that there is not a link between sex and failure of arthroscopic repair.
Several past studies have looked at characteristics of the rotator cuff tissue that may result in poorer outcome of repair. Gladstone et al (2007) found that fatty infiltration and atrophy of the rotator cuff muscles have a significant role in the outcome of repair. Atrophy and fatty infiltration were seen to progress even in tears that were successfully repaired, although in repairs that failed infiltration progressed significantly more. The authors of this study suggest that repairs should be performed promptly and if possible before there has been significant deterioration in the cuff. This study also found that tear size played the biggest role in determining the integrity of the repair.
Favard et al (2007) reported that when tendons of the cuff are torn the direction of their fibres are said to change, amount of muscle tissue decreases, and fatty infiltration and fibrosis of the muscle occurs. They suggest such changes may lead to increased difficulty repairing the torn cuff and may lead to poorer patient outcomes.
Nho et al (2009) found that multiple tears, co-existent biceps pathology requiring tendonesis, acromioclavicular joint pathology and poor quality of tendon tissue led to greater degeneration of the cuff and a higher incidence of persistent defect after surgery. Favard et al (2007) noted that factors that led to failure of tendon healing were age older than 65 years, fatty degeneration and delamination of neighbouring tendons. They also noted that better outcomes were seen in patients under 65, with small tears to the non-dominant arm.
The results of this study have not found a statistically significant relationship between tissue quality and outcome of repair. Additionally when looking at the group with tissue that is 'intermediate and delaminated' our results refute that tissue leads to a poorer outcome, especially when looking at the Oxford Score.
Furthermore in the follow-up phone calls the patient with tissue that was recorded as degenerative intaoperatively actually reported having a very successful repair. In fact the patient described the shoulder as 90% improved, which was reflected in the 3month and 1 yr Constant scores and the 3 and 6 month Oxford scores.
A study by Sherman et al (2008) looking at risk factors for revision rotator cuff repair found that older age and a large number of patient co-morbidities significantly influenced the outcome of primary repair. My findings definitely do not agree that age had a significant effect on operative outcome and in fact the results show comparable results for patients over and under 65 years of age for both outcome measures. In fact the majority of patients who required revision surgery were under the age of 65.
Biceps tendonitis and tears often occur at the same time as rotator cuff tears as part of the impingement syndrome or due to degenerative change. If pathology of the biceps tendon was present then the senior surgeon routinely repaired it at same time as rotator cuff repair. A study by Romeo et al (1999) found that co-existing rupture of biceps tendon, older age and tear greater than 5cm led to poorer postoperative outcome.
On statistical analysis of our results there was no significant association between treatment to biceps tendon and outcome at 3 months therefore I do not agree that there is an association.
It has been deliberated whether cigarette smoking has an effect on the outcome of rotator cuff repair.Nicotine is a known vasoconstrictor thus may have an adverse affect on tendon healing, especially in poorly vascularised regions such as near the insertion of the supraspinatus tendon. Mallon et al (2004) looked at the effect of smoking on the results of rotator cuff repair and found that smokers had significantly worse outcomes after repair than non-smokers and that fewer smokers had good or excellent results on shoulder assessment and less improvement in postoperative pain scores. Interestingly this study found that smokers also had poorer pre-operative shoulder scores despite there being no significant difference between the smoker and non-smoker groups in terms of age, gender, tear size etc. A study by Razmjou et al looking at outcome of repair also found that smokers had more functional limitations due to their shoulder than non-smokers.
Our results however did not show a statistically significant association between smoking status and outcome of repair although we could only find out the smoking status of the 48 patients that completed the questionnaire and out of these patients only 3 were current smokers.
A study by Bell (2004) found that patients who were likely to have retears and thus require revision surgery were those who had larger tears and those with poorer quality tissue and/or considerable retraction were also noted to have poorer outcomes.
Ide et al also reported that the incidence of patients with recurrent tears was significantly higher in patients who had severe tendon retraction than those who only had mild or moderate retraction. This study also reported that older patients had a greater incidence of retear.
Our results did not show an association between tendon retraction and post-operative outcome.
Individual patient outcome after RC repair strongly relates to how strictly that individual follows the rehabilitation protocol, wear their brace, and if they wait a sufficient period of time before returning to work and recommencing activities of daily living including housework and sports. These factors influence tendon healing and excessive activity may harm the arm further. All of the patients involved in our study were given a strict rehabilitation protocol to follow and a shoulder brace. Hopefully all our patients followed to this protocol and as non-adherence could have had an impact on patient outcomes.
The routine practice of the senior surgeon is to discharge patients who are recovering well to the care of the physiotherapists 3 to 6 months postoperatively and those who have less improvement may require longer follow up. As a result 3 months was the time at which most follow up data was available. The later data available (6months and 1 yr post-operatively) therefore shows some lower mean shoulder scores than the earlier results. However the current shoulder scores are higher on average and perhaps this just highlights that patients' heal at different rates and some patients may naturally take longer to recover from surgery.
No variables were found to significantly predict poorer outcome in current Oxford or Constant score, this may be due to the fact that most of these patients had good results and had potentially completely recovered from the surgery regardless of the degree of the initial injury.
The Oxford and Constant scores were our 2 outcome measures used to determine success of surgery but our results were consistently better using the Oxford rather than the Constant score and there were more patients with good/excellent Oxford than Constant scores. This may be due to differences in the 2 questionnaires; the Oxford score is a more subjective method of analysing outcome than the Constant score. The Oxford score is entirely a patient reported outcome measure (PROM) which means it can easily be completed by the patient at home without the need to attend the clinic. It is a joint specific questionnaire that was devised to give a representation of the patient's perspective rather than the entirely clinician-assessed scoring systems which existed previously and minimises potential biases that may occur when surgeons report their own patients' outcomes (Dawson et al 2009). The Oxford score has also recently been used as the primary outcome measure in a United Kingdom randomised controlled trial looking at the management of rotator cuff tears, including arthroscopic repair) that is being funded by the U.K. Department of Health (Carr et al, as cited in Dawson 2009). This emphasises that it is a trusted outcome measure that gives a reliable measure of patient satisfaction.
As the Constant score involves objective measurements of strength and range of movement as well as subjective questions, there is potential for differences between instrumental measurements of strength or professionals observing R.O.M. which could potentially bias outcomes. The Oxford score has been shown to be comparable to Constant score therefore should not be dismissed because scores are comparatively better. However I do think that the Constant score is a very good method of shoulder assessment as strength does play a huge role in patient satisfaction and has a major influence on how satisfied patients are with their repair.
Conclusion
The results of the audit show that arthroscopic repair of the rotator cuff by the senior surgeon achieved a large number of good/excellent results and significant improvement in patient outcomes from pre-operatively that continued over time.
Additionally our patients reported >80% improvement in shoulder function since the operation both at last follow-up and currently.
Tear size was a borderline significant predictor of outcome and I suggest that further research be done into it as a potential predictor of outcome to perhaps confirm the association.
References
• Flurin P-H., Landreau PD., Gregory T., Boileau P., Lafosse L., Guillo S., Kempf J-F., Toussaint B., Courage O., Brassart N., Laprelle E., Charousset C., Steyer A., Wolf EM. 'Cuff Integrity After Arthroscopic Rotator Cuff Repair: Correlation With Clinical Results in 576 Cases' The Journal of Arthroscopic & Related Surgery, Volume 23, Issue 4, Pages 340-346
• Boileau B., Brassart N., Watkinson D., Carles M., Hatzidakis AM. ,Krishnan SG. (2005) 'Arthroscopic Repair of Full-Thickness Tears of the Supraspinatus: Does the Tendon Really Heal?' Journal Bone Joint Surgery (Am.) 2005;87:1229-1240
• Gartsman G., Khan M., Hammerman SM. (1998) 'Arthroscopic Repair of Full-Thickness Tears of the Rotator Cuff' Journal of Bone & Joint Surgery; 80 (6): 832. (1998)
• Bishop J., Klepps S., Lo IK., Bird J., Gladstone JN., Flatlow EL (2006) 'Cuff integrity after arthroscopic versus open rotator cuff repair: A prospective study' Journal of Shoulder and Elbow Surgery; Volume 15 Number 3 2006
• Lugo R., Kung P., Ma CB. (2008) 'Shoulder Biomechanics' European Journal of Radiology 68 (2008) pages16-24
• Moosmayer S., Smith HJ., Tariq R., Larmo A. Prevalence and characteristics of asymptomatic tears of the rotator cuff: AN ULTRASONOGRAPHIC AND CLINICAL STUDY Journal Bone Joint Surg Br. 2009 Feb;91(2):196-200.
• Beaudreuil J., Bardin T., Orcel P. ,Goutallier D. (2007) 'Natural history or outcome with conservative treatment of degenerative rotator cuff tears' Joint Bone Spine 74 (2007) 527-529
• de Jesus JO., Parker L, Frangos AJ, Nazarian LN.(2009) 'Accuracy of MRI, MR arthrography, and ultrasound in the diagnosis of rotator cuff tears: a meta-analysis.' American Journal of Roentgenology 2009 Jun;192(6):1701-7
• Burkhart SS., Danaceau SM. and Pearce CE (2001) 'Arthroscopic rotator cuff repair: Analysis of results by tear size and by repair technique-margin convergence versus direct tendon-to-bone repair' Arthroscopy: The Journal of Arthroscopic & Related Surgery
Volume 17, Issue 9, December 2001, Pages 905-912
• Mallon WJ., Misamore G., Snead DS., Denton P. (2004) 'The impact of preoperative smoking habits on the results of rotator cuff repair' Journal of Elbow and Shoulder Surgery 2004; 13, Pages 129-32
• Romeo AA., Hang DW., Bach BR., Shott S. (1999) 'Repair of Full Thickness Rotator Cuff Tears: Gender, age and other factors affecting outcome' Clinical Orthopaedics and Related Research; 367 pages 243-255.
• Gumina S., Di Giorgio G., Perugia D., Postacchini F. (2008) 'Deltoid detachment consequent to open surgical repair of massive rotator cuff tears' International Orthopaedics, 2008 February; 32(1): 81-84.
• Dawson J., Rogers K., Fitzpatrick R., Carr A. (2009) 'The Oxford Shoulder Score Revisited' Archives of Orthopaedic Trauma Surgery, 2009, Volume 129 Issue 1: pages 119-123
• Constant C.R, Murley A.H (1987) 'A Clinical Method for functional assessment of the Shoulder' Clinical Orthopaedics, 1987 Issue (214):Pages 160-4
• Dawson J, Fitzpatrick R, Carr A. (1996) 'Questionnaire on the perceptions of patients about shoulder surgery.' Journal of Bone and Joint Surgery (British) 1996 July;78(4):593-600.
• Lee, E.W. and Flatow, E.L. Turek's Orthhopaedics Princilples and Their Application, 6th Edition, 2005, Lippincott Williams & Wilkins: Chapter 12- The Shoulder and The Arm
• Bell, R.H (2004) 'Arthroscopic repair of the rotator cuff' Master Techniques in Orthopaedic Surgery: The Shoulder, 2nd Edition, Lippincott Williams & Wilkins: Chapter 3, Pages 35-57.
• BMJ Best Practice: Rotator Cuff Injury, www.bestpractice.bmj.com
Acknowledgements
I would like to thank my supervisor Professor Funk for his help and guidance with this project. I would also like to thank Will, Sarah and Kat at the Bridgewater for their help collecting data and sending out questionnaires. I would also like to thank Jackie at Wrightington for her help accessing the NHS patients.